Sweden’s separate way of dealing, or rather of not dealing with coronavirus and COVID-19 pandemic has been widely criticised. While the Swedish government seem to be slowly reconsidering its approach, some Swedish scientists decided to voice their protest about the current policy which they say will cost many lives.
The authors of the following appeal are the Karolinska Institutet clinical epidemiologist Nele Brusselaers as well as biochemist Lynn Kamerlin from Uppsala and biophysicist Pernilla Wittung-Stafshede from Chalmers University of Technology. My readers will recognise Kamerlin as the organiser of the rather successful protest campaigns against the open access mandate of Plan S (read here, here and here).

Open Appeal:
As the Death Toll in Sweden Increases, Evidence-Based Policy Should be the Foundation of how We Address the COVID-19 Pandemic
(06 APRIL 2020)
COVID-19 has been spreading like wildfire around the globe.
Almost a month ago, the World Health Organisation (WHO) declared COVID-19 (disease due to infection by SARS-CoV-2 virus) to be a pandemic on March 11, 2020, when over 100,000 cases were reported globally in than 114 countries, and with more than 4000 people having lost their lives.
Since the declaration of a pandemic, over 1 million people have been confirmed to have been infected by this virus, with the actual number likely being much higher due to both limited testing in many countries, as well as the existence of many asymptomatic cases (the proportion of asymptomatic vs. symptomatic cases remains a matter of debate, however). In just a month, 4000 deaths has increased to over 70,000 deaths, and this number will likely increase substantially before things start to improve on a global scale.
Infectious disease prediction models have been used for decades to predict how fast epidemics are spreading, and to estimate which measures are effective in reducing the number of people becoming infected – and the number of people needing medical care, hospitalisation and/or a funeral. In other words, such models are critical in order to help predict the worst-case scenarios, and to get prepared to best tackle them.
Many countries have taken enormous measures to stop the spread of this pandemic, and have prepared themselves for large surges of COVID-19 patients. Measures taken already since mid-March include countries entering lockdown, banning gatherings, closing schools, banning visitors from early care homes, and enforcing social distancing policies in society.
In Sweden, a different direction is being taken in that rather than introducing strict bans, instead recommendations were formulated by the Public Health Authorities (Folkhälsomyndighet, FHM). These include:
- A proposal to the government to restrict public gatherings with more than 500 participants (March 11).
- Recommending staying at home when one is sick to avoid close contact with other people, and washing hands carefully to slow infection spread (March 16).
- For elderly (70+) to limit social contacts, and for employers who can, to let employees work from home (March 16).
- Recommending that colleges and upper secondary schools move to distance education _(March 17)
- To reconsider if the trip one plans to take is really necessary (March 19).
- To introduce new rules that restaurants, bars and cafés across the country avoid crowding at tables, buffets and counters, and that all service should occur at the table. Patrons are allowed to order and pick up their food and drink themselves only in so far as it is possible to do so without crowding (March 24).
- A further reduction of public gatherings from 500 to 50 participants (March 27).
As of April 1st, the most recently updated guidelines are that those who are symptomatic should stay home, to be careful with hand hygiene, and to follow social distancing practices. All operations in Sweden are responsible to, following FHM guidelines, take action to reduce the risk for infection spread. This can be informing the public, avoiding large gatherings, marking distances in queues, and offering the opportunities to wash hand with soap and water. Specific guidance is provided to shops, sports clubs, non-profit clubs and organizations, employers, and public transport, to follow guidelines for avoiding crowding, and to postpone unnecessary meetings and events.
Clearly, these are commendable guidelines that should be followed carefully by all involved. However, until today (April 6th), FHM has yet to clearly communicate that one should stay home if one has been in close contact with individuals with confirmed or suspects SARS-CoV-2 infection. In addition, there are no guidelines in place that one should identify close contacts if one is diagnosed with COVID-19, as advised by the World Health Organization (WHO) and supported by scientific evidence (see below).
Operating on guidelines rather than regulations requires a large amount of mutual trust between the public and the expert authorities, and Sweden is, in general, a country with reasonably high trust in the government.
However, a consequence of guidelines rather than regulations has been that there are still a large amount of people who are visiting bars, restaurants, shopping malls and, until recently, ski pistes, and this unfortunately is translating into a death toll that continues to climb in Sweden.
“Everything is under control” has been the main message from FHM, the governmental agency in charge of the COVID-19 outbreak, since the beginning of the outbreak – and to a great extent still is in early April 2020.
On the 27th of January, the “Statsepidemiolog” (State Epidemiologist Anders Tegnell) said that COVID-19 did not pose a threat in Sweden:
On March 14, the former State Epidemiologist (2005-2013), Annika Linde, argued that “letting the new coronavirus loose among children and healthy adults” would protect the older and those with multiple illnesses. (we note that, as discussed later in this piece, an increasing number of children and adults with no prior health complications have been becoming critically ill and dying of COVID-19; the disease is a threat for all societal categories).
This approach has been highly praised in the Swedish media:
This strategy, which resembles the one initially adopted by the UK government, can be summed up as ‘let the virus run through the population’. Effectively, this is a herd immunity strategy, which can be achieved either by allowing a large proportion of the population to be infected with the pathogen, or through vaccination. While a vaccine would clearly impart herd immunity, there remain simply too many open questions with regard to COVID-19 to try any other herd immunity strategy: how long does immunity actually last? Can you become infected more than once? Why do some people get so severely ill while others are asymptomatic, in particular if you compare two younger individuals, both not in risk groups or without other comorbidity factors?
This is not a disease that affects only the elderly or those in other risk groups, and considering the high case-fatality rate of COVID-19 (country-dependent, in the worst affected case, in Italy, over 12% according to Worldometer), there is likely going to be a very high death toll for this strategy as there is currently neither an effective treatment nor a vaccine for COVID-19. Following a report from a team at Imperial College outlining how large the loss of life could be if such a strategy where applied to the UK, the UK government changed course and is now taking strict suppression measures.
A death toll in the tens of thousands affecting all age groups would not be inconceivable in Sweden if such a strategy continues to be followed, due to the inherent risks of pursuing a herd immunity strategy with a highly deadly live pathogen/virus.
In addition, when the healthcare system is overwhelmed, this forces frontline medical personnel to have to make heart-breaking decisions about who can and cannot access care, as has been seen in Italy and elsewhere. This is a situation that should clearly be avoided in Sweden as far as possible.
What has happened in the previous weeks?
In response to concerns similar to ours, a petition was launched to entreat FHM to change its policy to come in line with WHO recommendations and the current state-of-the-art knowledge in the field. This petition was rapidly signed by 2000+ researchers affiliated to Swedish universities on 20 March 2020 and received broad media coverage in both national and international media.
Following likely at least in part due to a public request for an expert commission to advise the government, it was announced on March 31st, that such an expert panel would be installed.
It is good practice to inform public policy based on a group of independent and multidisciplinary scientists and doctors.
However, as of April 6th no further information has been provided on this front. We believe that it is absolutely critical that an expert panel with broad relevant expertise is installed as quickly as possible to support the public authorities. We are lucky in Sweden to have a large number of outstanding world leading virologists, immunologists, epidemiologists, and researchers with other relevant expertise to choose from. Their expertise is critical in this situation.
A famous Swede, Greta Thunberg, made headlines because she probably caught the virus (and was luckily doing fine) on March 24th. She used this as an opportunity to try to raise awareness of the risks this virus poses.
A young pregnant woman ended up on intensive care on March 27. Indeed, many reports of young patients dying from COVID-19, including infants and older children have come out.
Most countries observe and warn that COVID-19 can also severely impact patients under <50, in many cases even children, in many cases patients <50 without prior health complications, yet the focus of the Swedish strategy remains to be exclusively on protecting senior citizens and risk groups. While protecting the elderly and risk groups is important, all of society needs protecting, this virus is a threat to everyone.
In addition, the current Swedish approach fails to fully account for the fact that perhaps the greatest threat from COVID-19 is when the health system becomes overloaded or runs out of intensive care capacity (ventilators and the highly specialized staff for these). This is when the death toll starts to explode as seen in northern Italy.
International media started reporting about the situation in Sweden from around March 23-24. Scientists warned weeks ago that Sweden is playing Russian Roulette, an experiment with 10 million people.
In addition, despite the increasing evidence that the Austrian skiing town of Ischgl played a major role in facilitating spread of SARS-CoV-2 across Europe, Swedish ski resorts have remained open until April 6th, with reports of packed and humid après ski parties in many cases.
We note that the Editor of Dagens Nyheter, Peter Wolodarski, has been a vocal critic of the current FHM policy and the risks this poses to Sweden. For doing so, it has been argued in a major Swedish daily newspaper that he is contributing to “kunskapsförakt” (a term that is hard to translate directly, but essentially described as “contempt for knowledge”).
We re-iterate that it is absolutely critical for Sweden to follow an evidence-based policy approach in dealing with the COVID-19 pandemic, in line with the recommendations of major national and international organizations such as the WHO, the European CDC (ECDC) and others, as well as based on the rapidly increasing volume of scientific knowledge in this area. We appreciate that this is a rapidly changing area as we obtain new knowledge every day; however, it is critical to act before rather than after the virus, as the price of acting too late can be very high.
The Spanish flu in 1918 killed globally around up to 50 million people. A historical landmark epidemiological study from St. Louis vs Philadelphia showed that swift introduction of physical/social distancing measures saved lives and slowed the spread of the disease (Hatchett et al 2007, Caley et al 2007, Johnson & Mueller 2020).
So what is the current status now in Sweden?
Sweden is now still one of the countries with the most lenient approach in tackling this outbreak globally. Restaurants, bars, shopping malls are still open as of today – and gatherings up to 49 people are still allowed (last week it was still up to 499 people).
Since 1st of April, non-essential visits in elderly homes are however restricted, which is an important step in the right direction, but one that was unfortunately taken too late for the at least 50 elderly who already died in Stockholm.
It has in fact been estimated that roughly a third of residential care homes for senior citizens have been affected by SARS-CoV-2 with at least 400 residents infected as of April 2nd.
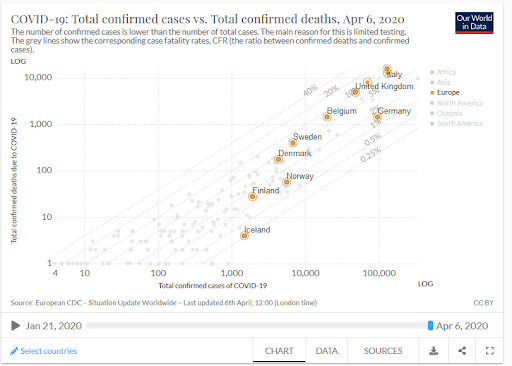
In Sweden, the first person died of SARS-CoV-2 on March 13th, which had already increased to over 500 people on April 6 (compared to 187, 73, 28, and 4 deaths in respectively Denmark, Norway, Finland and Iceland – noting that the number of deaths could be considered reflective of the “control” of the situation, independent of the population size – so we do acknowledge that Sweden is has the largest population in the biggest of the Nordic countries).
If this trend in Sweden continues at the current speed (doubling in 2-3 days, deaths at 4 days according to Our World in Data), Sweden will reach (the first) 1000 COVID-19 related deaths within days.
That is, as in many countries there is likely both a delay in reporting AND not all deaths have been confirmed as COVID-19, so they do not show up in the official numbers.
Recent estimates from the situation in Italy shows that the official death toll may be 2-3 times higher in reality. Excess mortality has been recorded as being very high for Spain and Italy; although the complete impact will only be clear once the pandemic is under control (https://www.euromomo.eu/)
We can only hope that there are not too many people yet who already died at home or without being counted (since COVID-19 may not be validated post-mortem), as the healthcare and testing has already been under (too) heavy strain for 3 weeks. In a few weeks, we will be able to assess the excess mortality (directly or indirectly related to COVID-19) through assessing overall-mortality in Sweden compared to previous years.
In addition, even at what is likely an early stage in the local pandemic progress, the health care system is already under extreme duress, especially in Stockholm, which is currently the Swedish COVID-19 epicenter.
What do we currently know about COVID-19?
The incubation time for COVID-19 – the time between exposure to the development of symptoms is between 2-14 days (outliers up to 27 days).
Transmission Pathways: The primary mode of transmission of SARS-CoV-2 is believed to be respiratory droplets and contact routes. However, it has been indicated that both aerosol and foamite transmission of SARS-CoV-2 is plausible, as the virus can remain viable and infectious in aerosols for hours, and on surfaces for up to days (depending on the inoculum shed). It was pointed out that the latter findings echo those with SARS-CoV-1, in which these forms of transmission were associated with nosocomial spread and super-spreading events (ibid).
Furthermore, a recent study identified a range of viruses (human coronaviruses, influenza viruses and rhinoviruses) in the exhaled breath and coughs of children and adults with acute respiratory illness. The authors noted that surgical face masks significantly reduced the detection of influenza virus RNA in respiratory droplets and corona virus aerosols, combined with a trend towards reduced detection of coronavirus RNA in respiratory droplets. These results were suggested to indicate that surgical face masks could prevent the transmission of human coronaviruses and influenza viruses from symptomatic individuals.
Transmission time: We know that mild cases are symptomatic for approximately 2 weeks; severe or critical cases 3-6 weeks; and that it takes approximately 1 week to develop severe disease (hypoxia). Most patients who died from COVID-19 died 2-8 weeks after onset of the symptoms.
People with COVID-19 could be infectious 1-3 days before developing symptoms and COVID-19 infected individuals could be asymptomatic.
This means that any interventions to limit the number of deaths will not show any effects before 2-14 days + 2-8 weeks; yet the effects may be visible sooner on the number of diagnosed infections.
As Italy shows, there are also great risks associated with delaying lockdown once there is widespread community transmission.
Who is most at risk for severe disease: Elderly especially living in care-facilities (high risk of transmission), people with asthma or other chronic lung diseases, or other underlying diseases including diabetes, obesity, heart problems, and immunocompromised patients.
However: there is increasing evidence of previously healthy younger individuals requiring intensive care following COVID-19 infection. Data from the CDC suggests that adults in the 20-44 age range have accounted (as of mid-March 2020) for nearly 30% of total USA COVID-19 cases, and 20% of the related hospitalizations. This number gets even higher once including adults aged 45 to 54 (50% cases and 40% hospitalizations). This is in agreement with warnings that suggest both an increasing number of younger patients, and with more severe complications, as well as data from France that raises the alarm that roughly half of critical cases in the ICU are patients under 60 years of age. It should be noted that there have been by now numerous deaths of young people with no prior health complications.
Therefore while older patients and those with pre-existing comorbidity factors have higher risk of complications from SARS-CoV-2 infection, no age group is invincible, and this virus is a threat to all segments of society – and all people have valid lives… old, young, sick or healthy… and should have the right to healthcare.
Could we have seen this coming?
Prediction models have been published specifically for Sweden:
Rocklöv’s group from Umeå: published online March 23, 2020
And it did reach the media, even if they did not present the worst- case scenarios – it should have been a wake-up-call:
Imperial College group (specific for Sweden):
And there is very convincing evidence that suppression methods are the only way to slow down the COVID-19 disaster, and that social distancing is not enough.
In the meanwhile, FHM have not shared their data and also apparently don’t believe in the value of such epidemiological prediction models.
How prepared was the Swedish healthcare system for a pandemic of this scale?
According to the Organisation for Economic Cooperation and Development (OECD), “Sweden has excellent healthcare but must improve care coordination”
Yet, in the same report, they also state that “coordination of care for patients with complex needs is less good”; “However, municipalities are often not adequately equipped to manage patients coming out of hospital so soon “
This should have been an alarm bell, considering how bad the situation quickly became in other countries such as Italy, China and Spain.
Prior to the COVID-19 pandemic, only Portugal had fewer intensive care unit beds per capita in Europe, with Germany having 6 times more intensive care unit beds per capita than Sweden (Rhodes et al 2012).
And recently not so positive news about preparedness for emergency care situations (although focussed on surgical emergencies)
“The Mass Casualty Incidents (MCI) preparedness of Swedish emergency care hospitals needs further attention. To improve Swedish surgical MCI preparedness a national strategy for trauma care in disaster management is necessary.”
Why didn’t Swedish authorities act earlier?
The COVID-19 outbreak developed rapidly in China in January 2020 – many people died, and the whole country went into lockdown. South Korea experienced problems following that, and then, already in early March, it became clear that the situation in Italy had deteriorated to the point that despite heroic measures, Italy could no longer contain the outbreak. All of these developments should have been warning signs for Sweden and other countries to act rapidly, as they watched the epidemic get out of control in highly developed countries with excellent healthcare systems in place.
Now, over 12,000 Italian healthcare workers been COVID-19 confirmed:
Over 2,400 have been admitted to intensive care units. Most European countries were in lockdown by mid-March. Meanwhile in Sweden, as of early February, FHM still criticized the idea of asymptomatic/pre-symptomatic transmission (and thus did not implement measures to address this risk). And by March 31, already 3 physicians and 2 nurses hospitalised at the intensive care unit in Sweden.
Public health advice by Swedish authorities:
- Family members of individuals who are high risk for COVID-19 should not stay at home (recommendation at least until end March))
- People are only advised to stay home once they are symptomatic, so individuals who are likely to have come in contact with infectious individuals are not recommended to stay at home (recommendation at least until end March) There are even reports that people are advised against self-isolation by official healthcare providers, AND not to mention this to contacts, since “it would only bring panic”.
- As of March 27, FHM also reduced the requirements for personal protective equipment (PPE) removing the requirements for a face mark and long sleeves (except for in very specific circumstances), which is dangerous as COVID-19 is a droplet infection, in fact community spread is likely mainly through droplet transmission and contact routes (understandably this move has garnered critique from healthcare professionals, see e.g. among others here, here and here).
This is very different to practice in other countries (while PPE is still available), where health care professionals are practically in “space suits”:
The World Health Organization (WHO) is clear in their recommendations for medical masks for health care personnel:
March 19: the WHO states that preventive and mitigation measures are key and “health care workers involved in the direct care of patients should use the following personal protective equipment: gowns, gloves, medical mask and eye protection (goggles or face shield)”.
Similar recommendations from the European Centre for Disease Control:
“Priorities for use of surgical masks: Those caring for COVID-19 patients, if no respirators are available. Symptomatic confirmed cases of COVID-19, followed by suspected cases”
Yet in Sweden, the PPE requirements have been reduced to not include masks as standard, which puts our healthcare professionals at grave personal risk at a time when we need them to be healthy and safe the most.
“The Swedish counties have new guidelines for personal protective equipment. They do not include a mouth mask….”
Although some hospitals still have and use better protection, there are many hospitals over Sweden, where healthcare workers are not allowed to use mouth masks – since they do not have any. And unfortunately, people are already dying in Sweden, as the healthcare system is becoming overloaded.
Finally, we note in parallel that while in Sweden they are reducing the PPE requirements for healthcare professionals, internationally, there is now also debate about extending the requirement for face coverings to the general public. For example, both Austria and the US now require or recommend some level of masks, either when attending public places like supermarkets (Austria) or as a general recommendation of cloth masks in public (US CDC).
Yes, it is important to avoid panic – but is it not better to be over-prepared?
As deaths in Sweden due to COVID-19 continue to increase, we entreat:
- The spread of COVID-19 in Sweden needs to be slowed down. As long as the tap is open, the water will keep running, and you will need more and more buckets to cope with all the flow. All large gatherings should be banned – a crowd is a crowd – if it is 499 or 49. All non-essential gatherings should be banned (restaurants, bars, shopping malls, etc.: not essential and dangerous)
- Stronger hygiene measures: frequent hand -washing with soap and hot water/both sides of hands, wearing a face textile cloth face covering (c.f. updated CDC recommendations, non-hospital/surgical level to avoid depleting healthcare system). Physical distance to other people is at least 2 meters (perhaps more indoors, this is subject to change currently as we know the virus is fully airborne).
- The healthcare system needs all the support before it completely collapses. Otherwise, even more people will die who could otherwise have been saved. Additional resources (beds, ventilators, drugs, personnel, personal protective equipment) need to be available to the hospitals now, and urgently.
- Our healthcare workers must be protected as much as possible, since they are daily risking their lives to save ours.
- Large-scale testing is crucial, to keep healthcare workers at work as long as possible; and to rapidly isolate those who are potentially infectious.
- Strict isolation and contact tracing: quarantine of everyone who tested positive for COVID-19 – not only once they become symptomatic. Everyone who came into contact with COVID-19 patients and has not been tested should go into isolation/self-quarantine for 2 weeks, as is practice in other countries.
“For mild laboratory confirmed patients who are cared for at home, to be released from home isolation, cases must test negative using PCR testing twice from samples collected at least 24 hours apart. Where testing is not possible, WHO recommends that confirmed patients remain isolated for an additional two weeks after symptoms resolve” (WHO)
- Get expert advice: Those in charge should listen to and assess available national and international scientific evidence on COVID-19. That promised expert council for Folkhalsomyndigheten should be up and running as fast as possible, and be truly independent, to support the work of FHM in developing evidence-based policy.
Undersigned are all scientists with relevant professional and personal experience considering the current COVID-19 outbreak in Sweden.

Nele BRUSSELAERS, MD PhD, Clinical Epidemiologist

Lynn KAMERLIN, PhD, Computational Structural Biologist

Pernilla WITTUNG-STAFSHEDE, PhD, Chemical Biologist / Biophysicist

Simultaneously frightening, rage-inducing and deeply upsetting.
I hadn’t seen Sjödin and Rocklöv’s paper. That the press is unable to digest it and report on its ramifications is incredibly troubling.
How no-one at the FHM or the government can see the urgent need for a red group is staggering. Not advisors. A red group..
LikeLike
A comparison of countries which are very similar, like Norway and Sweden, and where the covid-19 cases started at the same time is interesting:
LikeLike
Wouldn’t Switzerland and Sweden be very comparable as well?
LikeLike
Switzerland borders northern Italy, the epicenter of covid-19 in Europe. That alone makes it quite different. It is also different in many other ways, while Norway and Sweden are very, very similar, and are geographic neighbors.
LikeLike
Norway has more in common with Sweden. The population density in Switzerland is e.g. much higher. I have not been following Switzerland.
LikeLike
I live in Switzerland and I can say that the incidence of covid 19 cases, normalized over the Swiss population, is very high. The worst situation is in Canton Ticino, at the border with Italy and with a huge number of Italian workers (that is, people that live in Italy and work in Switzerland, and thus they cross the border every day). Now, in Canton Ticino they decided to have a lockdown similar to the Italian one: non-necessary activities, schools, bar and restaurants are closed. Over 65 people cannot go out. It seems to work quite well… Surprisingly, such decision was critized by the central Swiss government (Switzerland is a federal republic). Take also into account that Swiss health system is excellent but extremely expensive, there is not a public health system and all is based on compulsory health insurances.
LikeLike
So besides slowing down the contagion to prevent overloading the health care system, what else does supression actually provide? Does it really preserve a larger portion of the population from ever getting infected until the virus dies out, or the perspective is just to shut down everybody for years until a vaccine that may or may not be feasible be ready?
LikeLike
Fear mongering, misrepresentation and general nonsense.
LikeLike
What I am missing in most discussions is a connection to the estimation for ICU and hospital beds (skattning av vårdplatsbehov) by the Swedish public health agency (FHM), and how realistic their model is.
Click to access skattning-av-vardplatsbehov-folkhalsomyndigheten.pdf
(of course in Swedish)
Are Swedish hospitals prepared for this (as they say in the document) realistic worst case scenario?
Are Swedish authorities doing everything to avoid the worst case scenario?
Is the course of the pandemic in Sweden better than or at least equal to this worst case scenario?
Are Swedish authorities doing everything possible to follow the examples of the reference countries?
The answers based on gut feeling based on news articles is no, but I am yet to seen a scientific review of the document.
LikeLike
The question goes far beyond the scope mentioned here: all politicians must examine the global consequences of their decisions and in this case the number of collateral victims of heavy confinement could be a multiple of the direct victims of covid19
LikeLike
Pingback: Unmasking an opaque approach – Angies Schweden-Blog
I have to agree with the above article, Sweden doesn’t know better, and Anders’s “strategy” doesn’t hold water and can only work in a monopoly game.
Understanding the avoidance of panic and other stress that might come from tighter measures and isolation, this however cannot justify the current lifestyle during this pandemic.
Sweden doesn’t want to learn from the 200+ countries that have been through the same, and right now it’s sitting pretty much at the same level as Italy.
Italy imposed lockdown when they reached 1000 confirmed deaths(althought the numbers only account for tested individuals) and it was too late already.
How many deaths does Sweden need to understand that protecting it’s citizens should be top priority and that people are sometimes wrong(Anders T.) ?
Wake up politicians, start acting, trying to be “cool” “chill” and pretending you know best during such an event will only cost more human lifes.
LikeLike
Pingback: Шведский гамбит — p.com
Pingback: Failure of the Swedish model – OBJECTIVO
Pingback: Failure of the Swedish model – OBJECTIVO
Pingback: Sweden’s COVID-19 response | Green Left