This article lists all known (including those not officially declared) patients of the scandal surgeon Paolo Macchiarini, who received from him a cadaveric or plastic trachea. All these grafts were “regenerated” with bone marrow and epithelial cells, in some cases a bioreactor was used to incubate cells on the trachea carcass, in some cases a “bionic” method was applied, where cells were brought straight into the open patient, together with growth factors like EPO. Not all patients are named in my list, though names of all are available, certainly at the hospitals where they were treated. One of my sources is a patients list from the Careggi Hospital in Florence, Italy, which the Corriere Fiorentino journalist Alessio Gaggioli sent me. Some of the information comes from the 2015 “docu-novel” Megagrant, by Macchiarini’s Russian biographer and project manager.
This now is a full list, and it will be updated whenever I receive any new evidence. All Macchiarini trachea transplant patients are listed in the chronological order of their operation. The 2003 operated patient (story here), who received from Macchiarini (together with Heike and Thorsten Walles) a small “regenerated” tracheal patch of pig intestine, is not included here, as it was not a trachea transplant as such. There is a total of 20 patients, only 3 are known to be alive. Only one of them still has the graft.
Last update: 20.12.2023
- Claudia Castillo, born 1977, suffered from tuberculosis-damaged airways. Operated on 12.06.2008 at Hospital Clinic Barcelona, Spain. She received a cadaveric trachea graft which was implanted as a bronchus transplant, with the use of bioreactor for the purpose of regeneration. The organ was prepared without the knowledge of authorities in the veterinary lab of Martin Birchall at the University of Bristol, Macchiarini’s student Philipp Jungebluth was part of the process (see my report for details). The operation was published in The Lancet, Macchiarini et al 2008. A follow-up Lancet paper Gonfiotti et al 2014 reported the highly fragile patient travelling from January 2010 on for three years every 3-4 months from Barcelona to Florence, to be examined and to receive stents at Careggi, while always found in good health by Macchiarini and his partners. She was referred to Oriol Sibila at Hospital de la Santa Creu i Sant Pau in Barcelona in June 2013 by Jungebluth. Claudia’s real medical state was very serious at all times, due to infections and debris from poorly-biodegradable stents. she returned to Hospital Clinic Barcelona and asked to remove her left lung, which happened in 2016. She is now doing well, given the circumstances.

- According to a witness report (of another former Macchiarini patient), a 45-50 year old woman of a Middle Eastern origin was assigned to the private clinic BarnaClínic and operated by Macchiarini with a trachea transplant at the associated Hospital Clínic of Barcelona in the fall of 2008. She died at the ICU either around Christmas 2008 or in the first trimester of 2009. Hospital Clinic however was unable to find any records of a matching patient.
- D.D., female, born 1953. Diagnosis unknown (but likely no cancer). She was operated by Macchiarini on her airways twice before she was transplanted in October 2009 at Institut Dexeus in Barcelona. Prior to that, the Hospital Clinic forbade Macchiarini to transplant more patients (despite a queue), and now denies all knowledge of DD. Jungebluth was present at that operation, as part of his studies. This patient received a cadaveric trachea, which was smuggled from the Hospital Clinic, and according to Macchiarini’s lecture from 2010, was regenerated using so-called bionic method (no bioreactor) which Macchiarini developed together with his German partner Augustinus Bader (see my article here). In an unpublished manuscript however, Macchiarini claimed same bioreactor-assisted method as with Claudia Castillo was used (see here). The patient was afterwards emergency treated 13 times in thoracic surgery because of dyspnoea (difficulties of breathing) caused by collapse of the graft, “without final resolution”. A tracheostomy was opened in 2012, according to this unpublished manuscript, “due to severe laryngeal stenosis”. My source however stated that the graft detached soon after the transplantation, causing infection, tracheostoma was opened to save this patient’s life (read here). She likely died: in a 2014 lecture (min 12:30) Martin Elliott declared that “out of 10 patients worldwide” who received a cadaveric trachea “only 2 are alive”.

- Ciaran Lynch, born 2000 without functional trachea, received a homograft from Martin Elliott which functioned for 10 years. The boy received on 15.03.2010 from Macchiarini a trachea transplant (prepared in a lab at Royal Free Hospital, London, provenance however officially assigned to Italy) at Great Ormond Street Hospital in London. It was a cadaveric trachea in full, regenerated by bionic method (no bioreactor). Martin Elliott, but also Martin Birchall, were involved in the operation. Published in as Elliott et al, Lancet, 2013, a later follow-up as Hamilton et al 2015. See my article for details.

- M.K., female, born 1979, from Czech Republic, at the time mother of a 7 month old baby. She had mucoepidermoid carcinoma, was delegated to Macchiarini by her Czech doctor, the thorax surgeon Václav Jedlička. Operated at Careggi Hospital, Florence on 06.07.2010. She received a cadaveric trachea, using bionic method (no bioreactor). She also received chemotherapy in parallel. Sent home with mediastenitis (inflammation of chest cavity) on July 30th, later on fistula formation, cancer recurrence with the necessity of repeated bronchological interventions and chemotherapy was diagnosed, according to this Macchiarini-coauthored conference abstract (Jedlicka et al 2011). The patient died 1 year after diagnosis (which means already in 2010 or early 2011). Czech newspaper sources here and here. Clinicians directly involved at Careggi: Alessandro Gonfiotti, Massimo Jaus.
- Keziah Shorten, born 1991, from UK. She had adenoid cystic carcinoma and was operated on 13.07.2010 at Careggi, Florence, with a cadaveric trachea in full, regenerated by bionic method (no bioreactor). She also received intraoperative radiation therapy (IORT). The therapy was according to my information managed by Birchall; Macchiarini’s partner in the Careggi operation theatre was UCL surgeon Paul O’Flynn. The decision to perform the cadaveric trachea transplant in Italy was made at a multidisciplinary team meeting at UCL hospital on June 11th 2010. After the transplant failed, Keziah received from Martin Birchall a second transplant on 29.09.2011, Macchiarini was not involved (he allegedly even opposed this transplant). It was a plastic trachea, made at UCL and regenerated at Royal Free using a bioreactor. Keziah died in January 2012, she is mentioned as patient 2 in Culme-Seymour et al 2015. See my article for details.

- G.M, female, born 1987, diagnosed with left-side bronchomalacia (softness of bronchi). She was operated on 28.09.2010 at Careggi, Florence and received a cadaveric trachea graft to replace her left bronchus. Macchiarini’s clinical partners were Gonfiotti, Jaus. As severe complications with the graft ensued 2 months after the operation (aorto-bronchial fistula), she had her left lung removed and suffered “serious permanent brain damage”. Between 2010 and 2011 she underwent 7 interventions after transplantation (see also Corriere article). She likely died: in a 2014 lecture (min 12:30) Martin Elliott declared that “out of 10 patients worldwide” who received a cadaveric trachea “only 2 are alive”.
- M.M, female, born 1945, suffered from tracheo-oesophageal fistula, which happened postoperatively after larynx cancer treatment. She was operated on 04.10.2010 at Careggi, Florence with a cadaveric trachea, namely the cervical and media-trachea section. Macchiarini’s clinical partners were Gonfiotti, Jaus. The patient suffered then from venal thromobosis and infection of tracheostomy, transplant became necrotic and she died around one year after hospital discharge (see also Corriere article), according to this unpublished manuscript, in September 2012, “of sudden massive upper gastrointestinal bleeding”.
- Zhadyra Iglikova, born 1984. Russian patient who suffered tracheostomy after a car accident. She was operated by Macchiarini on 07.12.2010 at National Research Center of Surgery in Moscow and received a cadaveric trachea graft, namely cervical and mediastenic trachea section. Vladimir Parshin was Macchiarini’s operation partner. According to this unpublished manuscript, she received “a tracheoplasty with a T-tube” in April 2011, which suggest that the cadaveric graft was removed. An article by Dzemeshkevich 2015 described “graft’s stenosis due to scarring and granulation tissue formation without signs of preservation of native tracheal structure and function”. On 5.06.2018, Zhadyra received another cadaveric trachea transplant in Moscow (with no involvement of Macchiarini). She was sent home to Kazakhstan on June 24th and died on 8.07.2018. See my reporting here and here and this article in Filter.

- F.F., male, born 1938, diagnosed with squamous neoplasia of trachea. Operated on 25.01.2011 at Careggi, Florence, received a cadaveric trachea graft, in full, with neocarena. Macchiarini’s clinical partners were Gonfiotti, Jaus. The patient died very soon after, on 22.02.2011 (see also Corriere article), after “massive pulmonary embolism”.
- Danilo Bernandes Pedrosa, a Brazilian in Italy, born 1987, who suffered from a damaged trachea due to intubation after a car accident in 2009. According to local media reporting from April 2011, Pedrosa may have received a trachea transplant from Macchiarini at Careggi at around January 2011, having been transferred from a hospital in Pisa by his mother, “to follow the suggestions of doctor Macchiarini“: “In March, the boy seemed to recover, but before a new surgery for the change of the prosthesis to the trachea, Danilo deteriorated again.” He died on 2 April 2011. According to a Netflix documentary from 2023; Macchiarini entered a relationship with the victim’s mother to dissuade her from lawsuit, they even had a child.
- Andemariam Beyene, born 1973. Diagnosed in Iceland with mucoepidermoid carcinoma, operated on 09.06.2011 at Karolinska University Hospital, Stockholm. He received a plastic trachea made at UCL and bioreactor regenerated at Karolinska Institutet (KI). This and other bioreactors came from the company Harvard Apparatus (now re-branded as BioStage). Icelandic surgeon Tomas Gudbjartsson referred Beyene to Macchiarini, and was also participating in the operation. Philipp Jungebluth “regenerated” the trachea, took care of the patient and organised postoperative sample acquistion. Beyene died 30.01.2014, his story is told in Bosse Lindquist’s documentary “Experimenten“. Published as Jungebluth et al, Lancet 2011. See my reporting here and here.
- Christopher Lyles, born 1981, US American, diagnosed with adenoid cystic carcinoma. Operated on 17.11.2011 at Karolinska University Hospital, Stockholm. He received a plastic trachea made by Nanofiber Solutions (bioreactor regenerated). Involved was Philipp Jungebluth, who “regenerated” trachea and even operated the patient without a Swedish licence to practice medicine. Chris Lyles died on 5.03.2012. His family raised $200,000 for the operation. See my reporting here.

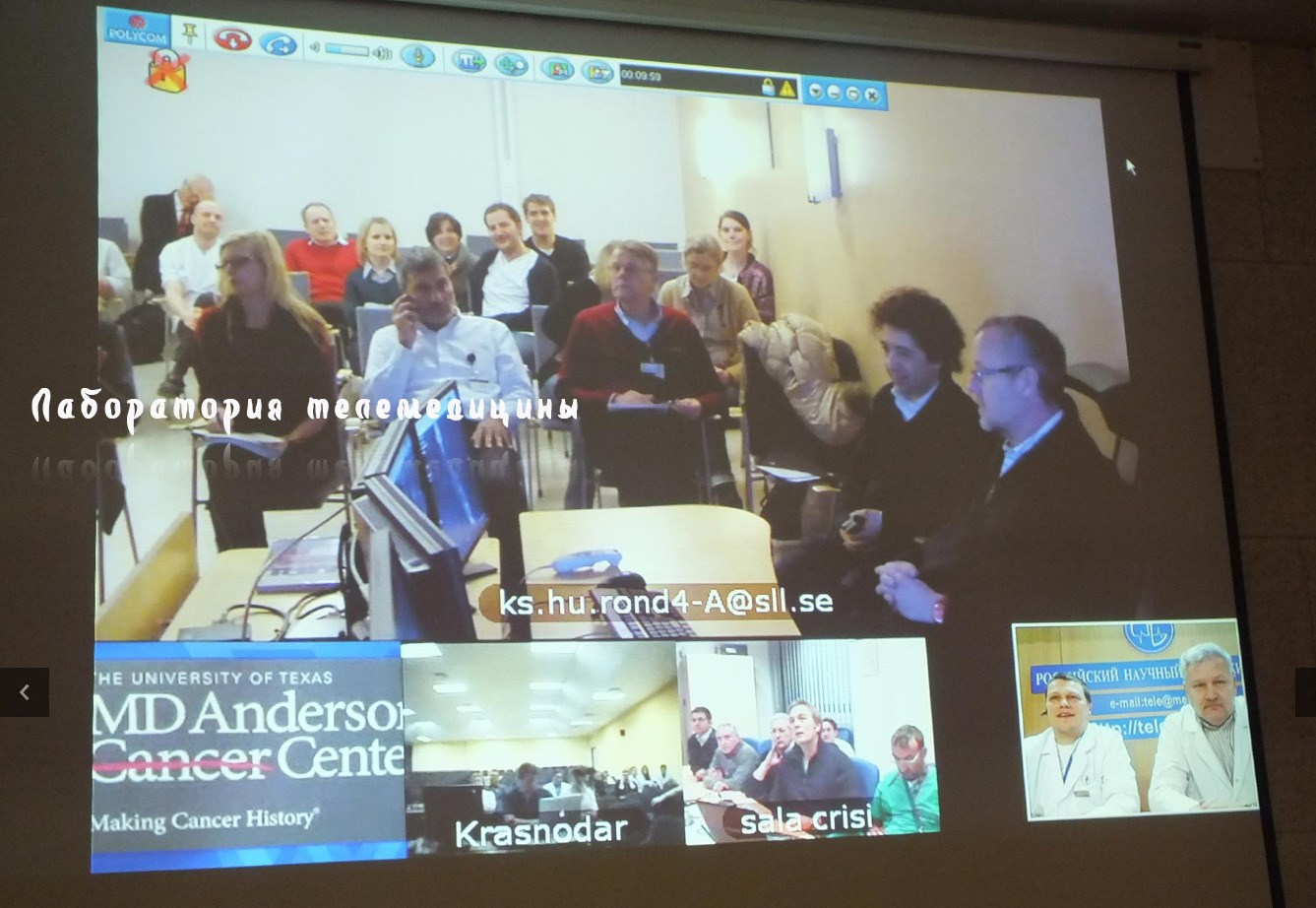
- Yulia Tuulik, born 1979, Russian, suffered from tracheostomy after a after car accident. Operated on 19.06.2012 at Kuban Medical University, Krasnodar. She received a plastic trachea from Nanofiber Solutions (bioreactor regenerated), and a second graft on August 2012. Macchiarini’s Russian surgery partners were Vladimir Porkhanov and Igor Polyakov. Philipp Jungebluth “regenerated” trachea and discussed operation). Yulia died in September 2014, her story is told in “Experimenten“. See also my article here and Alla Astakhova’s report.

- Alexandr Zozulya, born 1984, suffered from tracheostomy after car accident. This patient was an alcoholic and smoker, nevertheless operated on 21.06.2012 at Kuban Medical University, Krasnodar with a plastic trachea from Nanofiber Solutions (bioreactor regenerated). He received his second graft in November 2013. Macchiarini’s Russian surgery partners were Vladimir Porkhanov and Igor Polyakov. Philipp Jungebluth “regenerated” the trachea. Sasha Zozulya had several operations to improve his state, but died on 21.02.2014 due to mass bleeding, allegedly “from the area unrelated to trachea”, after “a bicycle accident” (referenced in Megagrant).
- Yesim Cetir, born 1990, Turkish, suffered from a damage to her trachea and lung drainage, after botched operation to fix hand sweating, but her quality of life was restricted. . Operated at Karolinska University Hospital, Stockholm, on 24.07.2012, where her right lung was removed, so a plastic trachea could be inserted on 7.08.2012. It was manufactured by Nanofiber Solutions and bioreactor regenerated. Yesim received a second plastic trachea graft on 9.07.2013, which was also removed. Philipp Jungebluth likely “regenerated” the plastic trachea, and transported a cadaveric trachea from Gothenburg as a possible replacement. Yesim died on 19.03.2017, after a lung-trachea transplant in Temple University hospital in Philadelphia failed to save her life. See also my reporting here and here.
- Hannah Warren, born 2010 born without functional trachea. The little girl was operated on 09.04.2013 at Children’s Hospital of Illinois with a plastic trachea from Harvard Apparatus. Macchiarini’s surgery partner was Mark Holterman, Philipp Jungebluth regenerated the trachea. Little Hannah died on 6.07.2013. She was supposed to be the very first plastic trachea recipient, but FDA repeatedly refused approval. Macchiarini then saw his previous plastic trachea patients as tests for Hannah’s transplant, and indeed, FDA eventually conceded based on those “successes” (referenced in Megagrant).

Children’s Hospital of Illinois, under fair use.
- Sadiq Kanaan, Jordanian. Born 1971, doctor by profession. Suffered from trachea stenosis due to complications from a 20 year-old trauma from car accident. Operated on 9.08.2013 Kuban Medical University, Krasnodar plastic trachea from Harvard Apparatus. Macchiarini’s Russian surgery partners were Vladimir Porkhanov and Igor Polyakov. Kanaan left Krasnodar a month after operation, allegedly against “prognosis” of surgeon Igor Polyakov. Died in 2014, according to Macchiarini on alcoholism (2015 book Megagrant), exact date unknown.

- Dmitri Onogda, born 1987, Ukrainian citizen of annexed Crimea. Suffered from tracheostomy after a car accident. Operated on 4.06.2014 at Kuban Medical University, Krasnodar, with a plastic trachea from Harvard Apparatus. Macchiarini’s Russian surgery partners were Vladimir Porkhanov and Igor Polyakov. Dmitri’s graft could be removed after 6 months when it started collapsing, he now lives with tracheostomy. See this RFEL report by Sergei Dobrynin.

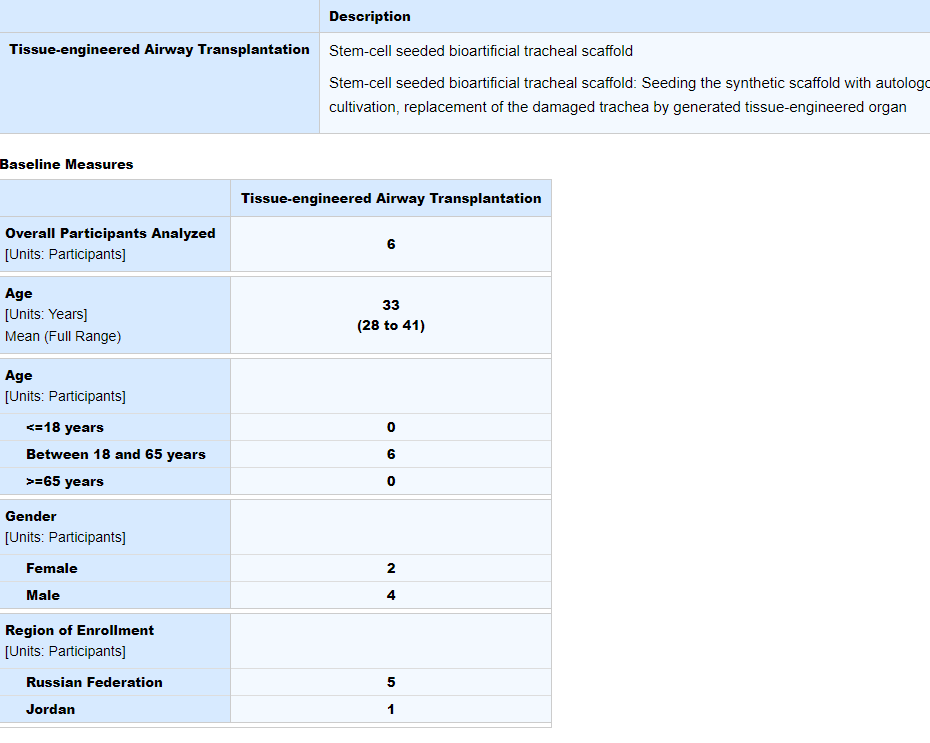
20. +21. Apparently, two more adult patients were operated in Krasnodar, male and female, both Russian citizens. Their names are currently unknown, as is their fate. Here is the evidence:
Records at ClinicalTrials.gov show that not 4 as officially known, but 6 adult patients received a plastic trachea transplant in Krasnodar: 1 Jordanian and 5 Russian citizens, 2 of them female. All are declared as disease-free survivors.
A conference report Weiss et al 2014 “Tracheal bioengineering: the next steps. Proceeds of an International Society of Cell Therapy Pulmonary Cellular Therapy Signature Series Workshop, Paris, France, April 22, 2014” tells about a presentation by Jungebluth at that meeting on results from Macchiarini group:
“Overall, the experience of this group has been that a number of deaths have occurred with both biologic and synthetic implants (8 of 18 patients have died). Many of these patients were seriously ill at the outset, including some with tracheal malignancies who had undergone previous treatment attempts. As such, most of the implants have been “ compassionate use ” in difficult clinical situations”.
Patient Onogda (Nr 19 above) was not yet operated when that Paris conference took place. Thus, he was apparently actually the last patient to receive a trachea transplant from Macchiarini (and 11th get a plastic one).
Was Onogda definitely the last? According to this report signed by Macchiarini, a 6-month old child “suffering from serious congenital defects” was operated on June 3rd 2014, “as a preparatory stage for the prearranged tracheal transplantation on the 28th of June 2014”. Nothing else is known about that child. Another Macchiarini patient had a close escape in early July 2014. A 20-year old Italian named Luigi, sufferer of trachea stenosis, was also supposed to receive a plastic trachea transplant in Krasnodar. Ethics permit “in Europe” was refused, according to his mother. An operation by Macchiarini and Porkhanov was reported to have left out the transplant, only a tracheoplasty was performed.
Several patients were operated by Macchiarini in cooperation with his former British partner, the UCL surgeon Martin Birchall. There was only one trachea transplant patient of Birchall’s where Macchiarini had no involvement: Shauna Davison (see here and here). The 15 year old girl received a cadaveric trachea transplant from Birchall’s partner Martin Elliott, on 15th February 2012. 12 patients received trachea transplants at that time point already, several were already dead. Shauna died on March 6th 2012, according to her obituary she suffocated when her new trachea collapsed. Birchall and Elliott however deny in their publications that her cause of death is known (patient 3 in Culme-Seymour et al 2015). They published this failed transplant experience as Elliott et al 2017.

A UCL investigation into trachea transplants revealed on September 30th 2017 that there was an 11th cadaveric trachea recipient: a 3-year old child, transplanted with the involvement of Martin Birchall in May 2017. Her current status was presented in the report as unknown (details here), afterwards Birchall, De Coppi and Elliott repeatedly claimed she was alive (Thakkar et al 2018, Elliott et al 2021, Ramaswamy et al 2023), read here:
Paolo De Coppi and the UCL organ factory
Paediatric surgeon Paolo De Coppi claims to grow all possible internal organs in his lab at UCL. Though his career started with his association with Macchiarini, and their regenerative medicine ideas sound strangely similar, De Coppi is celebrated as a modest genius poised to save lives of uncounted children, and the funding money flows.
Macchiarini also had collaborators at the University of Gothenburg in Sweden: the regenerative medicine researcher Suchitra Sumitran-Holgersson, and her surgeon partners Michael Olausson and Hasse Ejnell. Their primarily focus was “regenerated” blood vessels, but they also transplanted a decellurised trachea coated with patient’s bone marrow cells, on 2.03.2011. The elderly patient, whose diagnosis was tracheal stenosis, died 23 days later, the case is described here. The Gothenburg group also produced another decellurised trachea, which Jungebluth personally delivered to Karolinska for implantation in Yesim Cetir after her plastic graft failed. It was not used though. This experience qualified Olausson and Ejnell as experts advising the Swedish state prosecutor in Macchiarini case, with the result that all criminal charges against the former KI professor were dropped in October 2017.
I thank all my donors for supporting my journalism. You can be one of them!
Make a one-time donation:
I thank all my donors for supporting my journalism. You can be one of them!
Make a monthly donation:
Choose an amount
Or enter a custom amount
Your contribution is appreciated.
Your contribution is appreciated.
DonateDonate monthly


typo in ‘Patient 17’
firmer should be former
LikeLike
Pingback: Expert review: Macchiarini papers on plastic trachea transplants are misconduct – For Better Science
Completely unethical to publish images of patients with full names and presumed history without any consent.
LikeLike
all named patients agreed to be named, mostly in the context of advertising Macchiarini’s alleged successes. These patients were urged to go on camera, to promote their miracle doctors. This was of course perfectly ethical, I presume. All photographs are public domain, made so with patients’ or their family’s agreement. But I do agree, it is probably unethical to mention real human beings in a context which is disadvantageous to the treating clinician.
LikeLiked by 3 people
Pingback: Walles misconduct investigation in Würzburg widens inside a federal cover-up; Jungebluth’s dissertation whitewashed in Hannover – For Better Science
She seems a quite interesting girl with a lot of GRE/EU connections and a desire to run for office.
Greek Transcript for anyone who wants to do a better translation than mine:
Tatiana Stefanidou:Εσύ λοιπόν, έφυγες για μεταπτυχιακές σπουδές, κι εκεί άρχισες να διαπρέπεις στο εξωτερικό, να ανθίζεις εκεί, λοιπόν, πού πήγες και σπούδασες;
Eleni Antoniadou: Στην αρχή πήγα στο Λονδίνο, στο πανεπιστήμιο του Λονδίνου, στο UCL,έκανα μεταπτυχιακές σπουδές στη νανοτεχνολογία και την αναγεννητική ιατρική. Κι εκεί άρχισα να δουλεύω στο νοσοκομείο, στο Royal Free Hospital, όπου είχαμε και τη δυνατότητα να εφαρμόσουμε τις πειραματικές αυτές μελέτες σε ασθενείς που ήταν σε τελικό στάδιο καρκίνου. Και με διάφορες διαδικασίες που ήταν αρκετά δύσκολες, γιατί δεν υπάρχει νομικό πλαίσιο και δεν υπάρχει και δεν υπάρχει μια κλινική οδός στην οποία μπορεί να βαδίσει οποιοσδήποτε ασθενής σε οποιοδήποτε μέρος του κόσμου, ήμασταν τυχεροί ώστε και μπορούσαμε να τις εφαρμόσουμε και έτσι αποδείξαμε και λίγο τη δυνατότητα αυτού του πεδίου.
Tatiana Stefanidou: Έτσι, λοιπόν, έφτιαξες, έκανες το πρώτο σου μεγάλο επίτευγμα, για το οποίο μίλησε όχι μόνο η Αγγλία αλλά και ο κόσμος. Έφτιαξες την πρώτη τεχνητή τραχεία μαζί με μία συμφοιτήτριά σου, για έναν ασθενή με καρκίνο. Τον θυμάσαι αυτόν τον ασθενή; Του έσωσες τη ζωή; Μίλησέ μας για όλη αυτή τη διαδικασία. Πώς φτιάξατε την τραχεία; Πώς αυτός ο ασθενής κατάφερε να ζήσει μετά από αυτό; Να αλλάξει η ζωή του;
Eleni Antoniadou: H τεχνική που χρησιμοποιήσαμε…υπάρχουν διάφορες τέχνικες για να δημιουργήσεις νέα όργανα. Πήραμε από τον ομφάλιο λώρο του… Εμ, συγγνώμη, από το μυελό των οστών μεσεγχυματικά κύτταρα και τα καλλιεργήσαμε στο εργαστήριο και δημιουργήσαμε ένα ικρίωμα, δηλαδή τη ραχοκοκαλιά του οργάνου ώστε να μπορέσουμε να προσομοιώσουμε τις βιολογικές, φυσικομηχανικές ιδιότητες αλλά και το σχήμα,τη γεωμετρία, αλλά και να μπορέσουμε να προσομοιώσουμε τη βιοσυμβατότητα, ώστε να μην υπάρχει πρόβλημα απόρριψης αυτού του οργάνου. Φυσικά χρησιμοποιούμε διάφορες τεχνικές, 3D printing, και διάφορες άλλες τεχνικές, ώστε να μπορέσουμε να δημιουργήσουμε το ακριβές αντίγραφο του οργάνου το οποίο πρέπει να μεταμοσχευθεί. Ήταν μια πολύ σημαντική εμπειρία για μένα, γιατί φυσικά είναι άλλο να εργάζεσαι σε ένα εργαστήριο και καθημερινά να πασχίζεις ώστε να έχεις θετικά αποτελέσματα και άλλο να βλέπεις ότι τελικά αυτό είναι θεραπεία. Ότι μεταφράζεται σε κάτι που έχει μια κλινική αξία και κάποιος άνθρωπος από κει που δεν είχε καθόλου πια ελπίδες για να ζήσει, γιατί είχε μόνο 2 εβδομάδες ζωής ο συγκεκριμένος ασθενής. Είχε κάνει όλες τις χημειοθεραπείες που επιτρέπονται στην Ευρώπη να γίνουν για τη δική του πάθηση, είχε καρκίνο της τραχείας και είχε κιόλας ένα μεγάλο ογκίδιο στην τραχεία του. Μόνο με δύο εβδομάδες ζωής δεν υπήρχε κάποια άλλη θεραπεία, γι’αυτό δώθηκε ως εξαίρεση η δυνατότητα να εφαρμοστεί η δική μας πειραματική μελέτη, γιατί όπως γνωρίζετε, οι πειραματικές μελέτες δυστυχώς παίρνουν πάρα πολύ μεγάλο χρονικό διάστημα για να γίνουν τελικά θεραπεία, τουλάχιστον 20 χρόνια. Επομένως, ο συγκεκριμένος ασθενής ήταν και λίγο τυχερός γιατί γνωριζόμασταν με τους θεράποντες ιατρούς του. Εμείς είχε τύχει να παρουσιάσουμε το συγκεκριμένο, τη συγκεκριμένη τραχεία σε ένα διαγωνισμό που είναι για τη μετάφραση των επιστημονικών μελετών στην κλινική πράξη και κερδίσαμε το πρώτο βραβείο και έτσι μας δώθηκε μια μικρή δημοσιότητα στην Αγγλία και έφτασε στα αυτιά του συγκεκριμένου ασθενούς και είχε τη γενναιότητα να πει ναι και πιστεύω δεν πρέπει να το έχει μετανιώσει πια.
Tatiana Stefanidou: O άνθρωπος αυτός λοιπόν ενώ είχε 2 εβδομάδες ζωής του έγινε μεταμόσχευση της δικής σας τραχείας, αυτής που εσείς οι δύο φοιτήτριες δημιουργήσατε στο εργαστήριο και τώρα ζει μια φυσιολογική ζωή;
Eleni Antoniadou: That’s true. Ναι.
LikeLike
ENGLISH
Tatiana Stefanidou: So, you left abroad for postgraduate studies, and you blossomed, you aced it. Where did you go and what did you study?
Eleni A.: Firstly, I went to London, at the University of London, at UCL, I studied nanotechnology and regenerative medicine. There, I started working at the Royal Free Hospital, where we had the opportunity to apply these experimental studies in patients who were in the last stage of cancer, and with different procedures, which were very difficult, because there is no legal framework and clinical route, which a patient could lead in any place of the world, we were lucky because we could apply them and prove the capabilities of this field.
Tatiana Stefanidou: So, you had your first big achievement, which became the talk of the town, not only in England, but in the whole world. You made your first artificial trachea with the help of your coursemate, for a patient with cancer. Do you remember this patient? Did you save his life? Talk to us about the procedure. How did you make the trachea? How did the patient managed to survive this? His life changed?
Eleni A: eee… The technique that we used…there are many different techniques to create new organs. We got from his umbilical cord… Ehm, sorry his bone marrow mesenchymal cells and we cultured them in a lab and then we created a skeleton of the organ, so we could simulate the biological, physicomechanical properties and the shape, geometry and simulate the biocompatibility so there will not be a problem of rejecting the organ. Off course we used different techniques such as 3D printing and different techniques, so we could be able to create the exact replica of the organ that needs to be transplanted. It was a really important experience for me because it is different to work in a lab and every day and try hard to achieve positive results and it is different to actually see that it is a therapy. That it is translated into something that has a clinical meaning and an individual from a point that had no chances in surviving. Because he had only two weeks left the specific patient he had already done all the allowed chemotherapies in Europe for his condition, he had tracheal cancer and a big tumor in his trachea. With only two weeks of life there was no other therapy, so he was given an exception and chance for our study to be implemented, because as you know experimental studies unfortunately require a long time before they are actually implemented into therapy, at least 20 years. Consequently, this patient was a bit lucky because we knew his treating doctors; we had given a presentation about this, this specific trachea, at a competition about translating scientific studies into clinical practice and we won the first prize, and then we were given some publicity in England, this caught the attention of this specific patient and he had the bravery to say yes and I think that he has not regretted that.
-Tatiana Stefanidou: So this man, while he had 2 more weeks of living, he had your trachea transplanted, this that you and your friend made in the lab and now lives a normal life?
-Eleni A: That is true. Yes.
link Interview Star Channel Greece, 12/3/2014
minutes 5.00-8.51
LikeLike
He got in touch with us and asked whether the artificial trachea could be used as a transplant. We were extremely guarded as we hadn’t yet held an in vivo trial,” said Antoniadou, adding that the patient was willing to take the risk and the surgery was successfully carried out a few months later.
“He often expresses his gratitude to use, but the feeling is mutual because my life changed as well,” said Antoniadou.
http://www.ekathimerini.com/149953/article/ekathimerini/community/greek-biomedical-engineer-receives-top-award-at-age-25
LikeLike
It seems that Eleni Antoniadou is more a photomodel than a real scientist. All these mentioned here about her seem to be true. What it struck me was her complete lack of compassion for the patient (Beyene) and his family who received the trachea she created and he died because of that. It is so cruel to say that he did not regret receiving the trachea when you know that he is already dead for more than 1 year. I do not want to say anything about the journalists who did not even check the story. It is also sick that this woman is promoted as a role model for children and young Greeks….she is the first Greek woman to have a Barbie doll dedicated to her.
LikeLike
She says : “I think that he has not regretted that”. My God this patient was already dead since more than one year, because of this trachea. This girl is revolting. She is a total fraud and still everywhere in the media telling her fairy tale. I just can’t believe it. I think she’s also a pathological liar about everything. This person is disgusting and the press is giving her everything. And as you said, she is now presented everywhere as role model for children, repeating everywhere “girls can really do everything in science” while she…just did nothing and took part in the death of a patient in one of the biggest scandals in medicine history. I have to throw up
LikeLike
Eleni, who, after graduating in biomedicine in her native Greece, participated in the first successful artificial trachea transplant on a late-stage cancer patient at the Royal Free Hospital in London during her master’s in 2009. https://www.cartierwomensinitiative.com/candidate/eleni-antoniadou
I also got involved in developing a business plan for an artificial trachea. I felt overwhelmed when it was successfully received by a patient. It was proof that tissue engineering could be applied in clinical practice. http://www.nature.com/nature/journal/v505/n7482/full/nj7482-251a.html
While in the medical school of the University College of London, I worked with my classmate Claire Crowley for Prof. Alexander Seifalian on the development of a tissue engineered trachea that was mimicking the properties of its real counterpart. This graduate project was the winner of the Translation to Clinic and to Commercialization of Nanotechnology Products Competition in UCL and was shortly after implanted into a 36 year old patient, Andemariam Teklesenbet, who suffered from late stage tracheal cancer. This case was the first successful artificial organ transplantation in the history of medicine and proved the potential that regenerative medicine holds for future transplantation therapies.https://academy.arc.nasa.gov/eleniantoniadou
After graduating in biomedicine, she participated in the first successful arti3cial trachea transplant operation on a late-stage cancer patient. http://www.friendsofeurope.org/media/uploads/2016/12/2017-FoE-FE-EYL-2017-class-Bios-3.pdf
Here she is now http://www.healthparliament.eu/who-is-who/president
With Seifalian she was publishing under the name E.V. Antoniadou now she dropped the V. In addition she uses the transplant as a short of marketing for herself. If you ask her any question regarding the Macchiarini case you will get blocked from her social media.
LikeLike
There is some random evidence that she was not even in the UK during that period. ( http://www.fulbright.gr/en/alumni/greek-alumni/alumni-speak/405-eleni-antoniadou )
UCL Msc in Nanotechnology and Regenerative Medicine, (2009-2010)
UIUC Msc in Tissue Engineering, (2010-2012)
UCG Bsc in Computer Science and Biomedical Informatics, (2005-2009)
The trachea project is Claire Crowley’s PhD project… Claire completed her PhD at GOSICH, ‘Design and Development of an Artificial Tracheal Replacement with Clinical Application’
http://www.ucl.ac.uk/ich/research/developmental-biology-cancer/stem-cells-regenerative-medicine/intranet_profiles/staff/claire-crowley
http://www.ucl.ac.uk/news/news-articles/1107/11070701
It would be interesting her to prove that she actually took part in the transplant. 1) She is marketing the hell out of it. 2) In the Greek tv interview Beyene was already dead when she claimed to have saved his life. 3) Claire Crowley whose PhD project was the same trachea keeps a low profile. 4) She was not even in the UK at the time.
Anyway quite strange person…
LikeLike
In Greece, they have a saying to a free translation would be “you get an education equivalent to the qualities of your teachers” (eg. Alexander Seifalian). Eleni Antoniadou has a fake CV. She says that she has a PhD from Illinois, although she just has a master (https://www.ideals.illinois.edu/handle/2142/42480). Seems like they expelled her from Illinois during her very first year. Generally, she has a master of copying other people’s achievements (https://bioengineering.illinois.edu/news/article/bioe-students-win-big-cozad-0)
LikeLiked by 1 person
Ok there is definitely something weird with this E. Antoniadou. She is absolutely everywhere in the greek media, always presenting herself as a “Nasa researcher”. But i couldnt find NOTHING on the internet. She claims to be a scientist, but there are no publication at all with her name.
I would like to understand and to write an article about that. This could be a total fraud and people have to know. She is presented as the best greek scientist and she does not disagree. That’s incredible. I’ve met some Greeks that started their studies with her at the university, she was one of the worst students so I really don’t understand. And yet she just gave her face to a new Barbie doll, the “women’s model/example dolls”.
I really think it’s time to put and end to this fraud
LikeLike
Here is the perfect Ken to this Barbie: https://gizmodo.com/the-fake-sex-doctor-who-conned-the-media-into-publicizi-1832711205
I would blame media though, it loves good looking pathological liars, just like Macchiarini.
Contact me if you have a story to tell!
LikeLike
Yep the hype around her in Greece these days is incredible… The french wiki page has been modified, in order to be less hagiographic. It seems that the english wiki page had not been accepted by the community after a huge discussion about this public personnality
https://wikivisually.com/wiki/Wikipedia:Articles_for_deletion/Eleni_Antoniadou
LikeLike
Recently, it seems like this has started to gain more public attention:
https://www.telegraph.co.uk/news/2019/09/18/woman-inspired-first-greek-barbie-accused-falsely-claiming-worked/
LikeLike
Pingback: Unpublished Macchiarini manuscript confirms 5 forgotten trachea transplant patients, Jungebluth’s surgery practice in Italy – For Better Science
Pingback: The one who asked questions: interview with Johannes Wahlström, by Alla Astakhova – For Better Science
Pingback: Hannover Medical School MHH: where doctor careers matter more than patient lives? – For Better Science
Pingback: Unpublished Macchiarini manuscript confirms 5 forgotten trachea transplant patients – For Better Science
Pingback: EU commemorates dead patients of Macchiarini & Birchall with a phase 2 trachea transplant trial TETRA – For Better Science
It looks like the Russian Ministry of Health finally may be taking a closer look at Macchiarini. “Russian authorities request information about Macchiarini”. (Swedish)
http://www.lakartidningen.se/Aktuellt/Nyheter/2017/09/Ryska-myndigheter-begar-ut-information-om-Macchiarini/
LikeLike
Pingback: Alexander Seifalian, UCL’s Persian Scapegoat – For Better Science
Pingback: Swedish police investigation acquitted Macchiarini on advice of misconduct-tainted trachea transplanters – For Better Science
Pingback: Swedish Central Ethics Review Board finds Macchiarini guilty of misconduct, requests retraction of 6 papers – For Better Science
Pingback: How trachea transplanters tricked Andemariam Beyene to sacrifice himself for a Lancet paper – For Better Science
Pingback: Cowboy Surgeon: A Story of How Expectations in Research Led to Tradgedy – Maddicinal Science