As we learned it from the Swedish documentary „Experimenten“, the scandal trachea surgeon Paolo Macchiarini didn’t much like to operate on sick cancer patients: they died too quickly after receiving a trachea transplant. This is why Macchiarini was said to have moved on to patients outside of any life-threatening conditions, like the Russian car accident victim Yulia Tuulik. She died because of the plastic trachea which Macchiarini implanted into her. Yesim Cetir, young victim of a botched operation, was slightly luckier to survive the plastic trachea, but only because it was removed and because of constant emergency care and multiple organ transplants (she is presently in very grave state). However, it seems that even Macchiarini’s cancer patients could have led a relatively long life, had they not agreed to receive his trachea transplants. And I am not speaking about the lethal plastic ones. In fact, the “biological” grafts made of decellurised dead donor tracheas were not such a great success either, and seem to have brought suffering and have shortened lives instead of prolonging them. The British UCL and its hospital UCLH are preparing their own clinical trial with cadaveric tracheas, while busily covering up their role in the Macchiarini scandal.
A manageable disease
From talking to specialists, I learned that there are basically two types of cancer of the trachea: the squamous cell carcinoma and the adenoid cystic carcinoma (ACC). The former is a very rapid and lethal cancer, which appears in older patients (mostly due to smoking) and which requires immediate and radical surgery to try and prolong the patient’s life. The latter, ACC, is a slow growing and according to medical literature very well manageable (though not curable) form of primary cancer, which is not related to smoking and occurs in young patients. The ACC is apparently exactly the type which almost all Macchiarini’s cancer patients, who received a trachea transplant, had. One patient, Andemariam Beyene, had prognostically an even more favourable form of cancer (see below). It is true that these cancer sufferers were indeed incurable and eventually faced death. It is another issue altogether how long they would have lived had they avoided that miracle doctor and chose traditional therapy instead.
With ACC of trachea, the patient’s airways are progressively obstructed by the tumour growth which can lead to suffocation if untreated. The traditional and well established options are either stenting (where the airways are dilated from inside by a balloon or a net), mechanical tumour scraping or laser surgery to remove growths, and finally resection (where a short constricted segment is excised). The cancer can also be treated by chemo- or/and radiation therapy (e.g., Allen et al 2006), but eventually it metastases into the lungs which then inevitably leads to death. However, compared to squamous cell carcinoma victims, ACC sufferers have a very good prognosis and 5-year median survival rate (Webb et al 2006), in fact even according to Macchiarini himself it is around 80% (Del Gaudio et al 2013, free full text here). The described therapy methods aren’t even novel and existed for more than 10 years (e.g., Howard et al 1994, Okahara et al 1996 or Aggarwal et al 1999) when Macchiarini started applying his exciting alternative of cadaveric trachea transplants to ACC patients in around 2010.
In view of this, removing trachea and replacing it with an artificial transplant (even if that transplant worked, which in case of Macchiarini can’t be really assumed) will do nothing to stop the cancer progress, and it will not help any with cancer-induced damage to the surrounding organs like the oesophagus. In fact, a replacement of trachea would be counter-indicative here, since it will not prevent metastases, but put the patient into under undue risk.

Did Macchiarini’s cadaveric trachea transplants help anyone breathe better? Most obviously not, every single such patient apparently required permanent stenting as not to suffocate, like Claudia Castillo or Ciaran Lynch (both patients operated with his former partner, Martin Birchall, now professor at UCL, and master of his own stalled trachea transplant trial). Both these patients are being constantly paraded by Birchall as successes of the cadaveric trachea transplant technology which he developed (the Macchiarini bit fell under the table, in fact Macchiarini was excluded from the authors list in The Lancet paper Elliott et al 2013 describing Ciaran’s transplant which the Italian miracle surgeon performed). When more and more evidence came out on the sad reality of Claudia Castillo’s case (constant emergency care and lung amputation), Birchall apparently dropped her as his evidence. In a conference talk in September, he admitted according to a member of audience that Claudia’s transplant was actually not a success.
The patients Castillo and Lynch had no cancer, this may be the only reason they are still alive. Not because of Macchiarini’s and Birchall’s cadaveric trachea transplant, but possibly despite of. But another young patient of theirs, Keziah Shorten, had a terminal cancer, and she died. Her story is told in the Bosse Lindquist’s TV documentary “Experimenten”, she is also mentioned in this publication by Birchall as patient 2 (Culme-Seymour et al 2015). I have some more details to add.
Keziah’s story
Keziah was 19 when her ACC was diagnosed, and a family contact in Italy brought her to be operated by Macchiarini at the Careggi hospital in Florence in 2010. Another ACC-suffering young woman, from Czech Republic and aged 31, whose name we do not know, was also operated by Macchiarini there (mentioned here). Keziah Shorten died in January 2012, also the Czech patient died, as indicated by this Science article from 2013: “Macchiarini says another adult patient also died of the cancer that had damaged the trachea” and by Macchiarini’s own publication (Jungebluth & Macchiarini 2014, free full text here). However, elsewhere the same miracle surgeon claimed in his summary for EU-funded (and soon terminated) clinical trial Biotrachea (awarded in April 2012):
“Based on our previous clinically successful experiences with in vivo completely tissue engineered tracheal replacement in benign tracheal diseases, we recently applied this technology in 2 patients with otherwise inoperable primary tracheal cancers. The successful observed outcome confirms the unique opportunity to scale-up an effective therapeutic approach into a widely accessible clinical technology, which could enhance not only the quality of life but even cure otherwise untreatable patients”.
Again, we know very little about the other patient, but the operation on Keziah Shorten was NOT a success. It was in fact a horrible and very tragic disaster. In July 2010 Macchiarini removed her constricted trachea and replaced it with a cadaveric one treated with his special stem cell magic. Apparently, like with Ciaran Lynch before and unlike with the initial patient Claudia Castillo, no bioreactor was used: the cells were just smeared onto the decellurised cadaveric graft while it was being transplanted. Macchiarini also treated Keziah with Intraoperative Radiation Therapy (IORT, details of this exact intervention: page 8, in Italian). Keziah went home to UK, where a first-hand source told me she was examined by “her British surgeon”, her graft was found to have “developed its own independent blood supply”. That would indeed be a major biomedical sensation, since no other Macchiarini transplant showed much in this regard objectively. Yet nobody bothered to announce this miracle to media. Who was this British surgeon? I was only told that it was not Birchall. Yet the Culme-Seymour et al 2015 paper declares that next to Birchall, the pediatric surgeon Martin Elliott was responsible for Keziah’s care: “M. J. Elliott and M. A. Birchall were the clinical leads for the three patients”. Elliott never replied to my email about Keziah’s operation. Elsewhere, Elliott still maintains publicly that his and Birchall’s patient 1, Ciaran Lynch, was a resounding medical success, despite their own published evidence to the contrary (Hamilton et al 2015). Their patient 3, who died right after receiving a cadaveric trachea transplant, was the 15-year old Shauna Davison.
In April 2011, Keziah’s cadaveric trachea transplant failed. In September 2011, she was operated at the UCL Hospital (UCLH) and received a plastic trachea, made by the nanotechnology specialist and then-UCL professor Alexander Seifalian. The operation was performed by Birchall in London, unlike with Ciaran Lynch before, Macchiarini was not directly involved. The transplant quickly failed as well, it separated at the base (just as it happened to another of Macchiarini’s first plastic trachea recipient Andemariam Beyene, who was transplanted a Seifalian-made trachea in Stockholm, in July 2011). By this time, Keziah already suffered from hospital-acquired pneumonia. She died in January 2012.
Changing the past
Seifalian was sacked from his UCL professorship in 2016 and seemingly assigned the entire blame for the failure of Macchiarini’s trachea transplants. Which may seem somewhat unjust, since Seifalian is not a doctor, he is not even life scientist by training. His professed ignorance about tracheas might be forgiven, up to a degree. Birchall, who is on the other hand a very eminent surgeon of the airways, now profusely distances himself from the knowledge of dangers of plastic transplants, and seems to receive full support from his employer UCL and UCLH. His REF2014 Impact Case Study report “The world’s first stem cell based transplants: changing the future of organ replacement” is not searchable anymore from the main page, even the keyword “Birchall” turns up nothing. It is understandable why, since the way Birchall presents his successes “to save the life” of Claudia Castillo and Ciaran Lynch may appear as not entirely sticking to truth. Also Shauna Davison operation was “successful”, her rapid death, unlike the never published “paper in preparation” went unmentioned. The references in that REF2014 report are somewhat wonky. This MRC “Achievements and Impact” page of radiantly smiling Birchall was removed (here a cached copy), also the REF2014 referenced BBSRC link about his new strategy in regenerative medicine leads nowhere. In January 13th 2016, my website was accessed from a strange source and right after all my relevant articles disappeared from Google search on “Martin Birchall”. Meanwhile, the search results are largely back.

Even a photograph of Birchall together with Seifalian happily holding a plastic trachea was purged from internet by UCL. The new UCL truth is: Birchall was always against plastic tracheas. Always.

In Culme-Seymour et al 2015, Birchall wrote retrospectively about his patients Keziah and Shauna:
“Patients 2 and 3 had significant co-morbidities at the outset, and whilst both unfortunately died, the causes appeared to be unrelated to the grafts. Prior to death, both patients had a high quality of life, albeit for short periods of time, and both would almost certainly have died much earlier if untreated”.
Is it really a “good quality of life” experience to lie in a septic fever while slowly suffocating on a detaching plastic tube inside your throat? Anyway, this is what Keziah’s surgeon Dr. Birchall wants us to believe here. In “Experimenten” however, he told something else (see transcript starting at 0384):
“The two ends of the trachea were very loose, they had not integrated at all. There were sutures holding it in place, but very loosely. She remained on the intensive care unit at UCL for another six weeks- but then was able to be discharged back to Brighton to be with her family for a few months. Keziah’s condition worsened, and shortly afterwards she passed away”.
So Keziah’s second plastic transplant never worked. What about her first, the cadaveric one, which apparently was the root of the catastrophe? As I evidence below, UCLH and thus possibly even Birchall himself were involved into approving her first disastrous trachea transplant in Florence.
Decision made in London?
An expert I spoke with told me that what actually caused Keziah’s death was the first transplant, the one made of decellurised cadaveric donor organ. After that failed, she was doomed. So who made that decision to operate Keziah with a cadaveric trachea and IORT at the Careggi hospital in Florence? The official version is that it was all solely Macchiarini’s doing, and UCL and Birchall tried to save her life then: “the patient then travelled to UCLH for post-surgery care” (Culme-Seymour et al 2015).
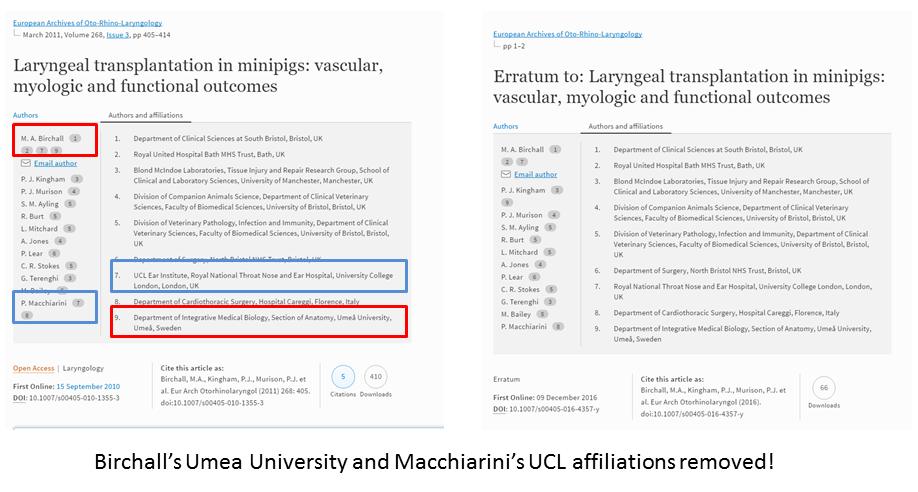
Yet there is a photograph of Keziah in her Careggi hospital room, surrounded by three doctors in scrubs (I don’t want to post it here, follow the link if interested). One on the left is Macchiarini, one on the right is an unnamed Italian doctor, the one in the middle is most obviously Paul O’Flynn. This UCLH doctor was taking care of Keziah when she was treated at UCLH, he is even mentioned in this obituary. What was he doing in Florence in summer 2010? I received information (below) that the Careggi operation was in fact approved in advance by the doctors comittee at UCLH, with Macchiarini likely present. He was namely honorary professor at UCL since November 2009 and until June 2014, honorary consultant at Great Ormond Street Hospital for Children (GOSH, the children’s hospital where Elliott works) and had admission and bronchoscopy privileges at The London Clinic. Now of course, Birchall and UCL work hard to remove all traces of Macchiarini’s professorship in London, for example, an Erratum to Birchall et al 2011 from December 2016 banished it into thin air.
A first-hand source insisted Keziah’s operation was financed by the British public health service provider NHS (which only could happen if the operation was approved in UK), yet NHS denied this to me:
“We have liaised with the relevant department within NHS England and can confirm that we have no record of receiving any request for a trachea transplant”.
However, NHS England did not yet exist back then in 2010. I asked NHS if they checked with the records of the respective Primary Care Trust but received no reply so far.
So what was O’Flynn doing in Florence? Was it a private visit to Macchiarini at his workplace, or was he sent there by UCLH? Who else went with him from UCLH and why? O’Flynn refused all communication with me. So I submitted a Freedom of Information (FOI) inquiry to UCLH, already knowing from past experience that I will not get an easy or truthful reply. I asked UCLH these questions:
- Why and in which capacity did Dr. O’Flynn travel to Careggi in regard to this operation?
- Who recommended this Careggi operation to NHS so it was paid by it?
- When did Paolo Macchiarini discuss this patient’s case with the multidisciplinary team at UCLH prior to the operation’s approval, and who was present from the UCLH side?
After almost a month, UCLH issued me with this reply:
“We are not obliged to respond to your request as we consider it to be vexatious under Section 14(1) of the Freedom of Information Act 2000”.
The definition of vexatious FOI requests is here, I am not sure how my inquiry falls into any of categories. But I do agree if UCLH was indeed involved in approving and overseeing Keziah’s catastrophic trachea transplant by Macchiarini in Florence, it would be a most unwelcome publicity for UCLH these days. The potential reputation damage to the venerated institution of UCLH, combined with possibly then unavoidable investigations by UK authorities, does indeed drive my insolent information request vexatious beyond any definition.

Italian Mysteries
Alessandro Nanni Costa, head of the Italian National Transplant Centre (CNT), shared some information with me about Keziah. According to him, the decision to operate Keziah with a cadaveric transplant and IORT was made at least in part by UCLH:
-
“The referenced patient, affected by primitive adenoid cystic carcinoma of the trachea has been treated with the transplant of a donor’s trachea after a clinical assessment performed by the Guy’s & St. Thomas Hospital, Head and Neck Centre at the University College London Hospital [this is where the Careggi visitor O’Flynn is employed as consultant surgeon, – LS] and by a multidisciplinary clinical and oncological team at the Careggi Hospital in Florence. The experts that have evaluated the patient’s conditions have proposed the surgical resection with transplant as the therapeutic treatment. The other traditional therapeutic options that were considered, namely the surgical treatment (total laryngectomy, partial pharyngectomy, total esophagectomy with gastric pull-up), have been considered not appropriate ;
-
before starting the treatment the clinical case and the protocol were submitted to the local Ethical Committee of the Careggi hospital; the latter expressed a positive opinion ;
-
considering the urgency with which the case had been submitted, the Italian National Transplant Centre (CNT) asked for a clinical protocol to be approved by CNT based on the positive opinion of the Superior Health Council that is the technical consulting Committee of the Health Ministry (Consiglio Superiore di Sanità), as foreseen by the Italian regulations;
-
on June 2011 the Superior Health Council released a positive opinion on that protocol;
-
the informed consent form for the patient, attached to the protocol, explicitly mentions the availability of traditional therapies; nevertheless these were considered by the physicians not applicable for the treatment of patients undergoing trachea transplant;
-
6) it is worthwhile to note that the authorizations invece di opinion: OK? released by CNT is concerning the regulatory classification of the therapy, which in the specific case is a tissue used for transplant. Decisions about other therapeutic options are not the responsibility of CNT but of the clinicians. They keep the competence to evaluate the clinical conditions of the patients and to choose the best treatment”.
There were in fact at least three patients operated by Macchiarini with cadaveric tracheas in Florence (we know already of Keziah and the unnamed Czech patient). These first two interventions were applied for by Macchiarini on June 7th 2010 to the Ethics Committee of the Careggi hospital, approved there on June 10th and authorised by CNT as compassionate use cases on June 16th 2010 (see original ethics approvals here), another compassionate use case followed them. One more of Macchiarini’s trachea transplant patients, also a young woman, is described in this Corriere Fiorentino article as suffering from January 18th 2011 on from severe complications, in particular very high fever.
Nanni Costa made repeatedly clear to me that his institution only approved the procedure as such and did not make any assessment for its medical applicability to each individual patient and her case; this was in fact decided by Macchiarini and his clinician colleagues at Careggi. When Macchiarini requested to operate more patients, CNT directed him to submit a proper application to the National Health Council in Italy, which Macchiarini and Careggi also did. As Nanni Costa explained, and which is confirmed by these documents:
“The Head of the Careggi hospital (Direttore Sanitario) has submitted the protocol to CNT on 23.11.10. On 1.7.11 CNT approved the protocol based on the positive opinion expressed on the 14.6.11 by the Consiglio Superiore di Sanità”.
Under this approved clinical trial only one single patient was operated, as confirmed by this Corriere Fiorentino article, where Nanni Costa is quoted. In fact, it seems Macchiarini operated more patients than officially recognised.
How many patients?
Yet another Corriere Fiorentino article by same journalist Alessio Gaggioli lists a total of 7 recipients of Macchiarini’s cadaveric tracheas: 2 operated in Barcelona in 2008-2009 (first one was Claudia Castillo) and 5 in Florence, four of them in 2010, last in 2011 (possibly that only patient of that Careggi clinical trial). This number was apparently officially reported by Macchiarini himself to the Tuscan authorities. Only one of these 5 Florence patients is said to be alive, with a “serious permanent brain damage”. According to the Barcelona clinic head Antoni Castells, that 2nd operation on a Spanish woman (who arrived from Dortmund in Germany) was cancelled and never took place in his hospital (see my report here). Yet even Macchiarini himself speaks of 9 patients in Jungebluth & Macchiarini 2014, which would make sense given that the extra two were operated elsewhere: namely Ciaran Lynch in London and Zhadyra Iglikova in Russia (see her sad story here and here).

Update 19.02.2017. At a February 28th 2011 networking event in UK, Birchall spoke of a total of 7 patients he transplanted with cadaveric organs, as follow-up to Claudia Castillo’s “life-saving – and life-transforming – operation”:
“Birchall told delegates that since then he has conducted six other replacement procedures, using donor organs that are de-cellularised and then seeded with stem cells and growth factors”.
Officially, Birchall only transplanted 3 patients with cadaveric grafts: Claudia, Ciaran, Shauna. Are those extra 4 his own (operated in secret at UCLH?) or in fact Macchiarini’s Careggi patients which Birchall ascribes to himself in the conference speech? If so, why? Was he involved into these Italian operations after all, just as the suspicion is emerging in regard to Keziah?
No plastic, no clinical trial!
Why did Macchiarini abort his clinical trial in Careggi? Apparently, he decided to switch to plastic tracheas. This is how Nanni Costa explained it to me:
“The Head of the Careggi hospital asked CNT on 29.3.12 if the use of nanosynthetic scaffolds could be used instead of the cadaveric trachea. CNT replied that for this change an amendment of the protocol had to be submitted again to CNT for a new approval, after a new CSS positive opinion. The amendment was never received”.
The star surgeon is well known for his tendency to rapidly change protocol. He used a bioreactor-made trachea on Claudia Castillo in 2008, then suddenly he switched to smearing cells onto the graft while transplanting it in 2010, on Ciaran and Keziah (possibly after that 2008 scare with the British authorities which I uncovered). He ran his own EU-funded clinical trial Biotrachea aground, according to my evidence solely because he refused to surrender his plastic trachea patent to Seifalian’s UCL and insisted on using an alternative plastic source where the patent issue was more advantageous to Macchiarini (see details here). So it is hardly a surprise that after the volatile Italian surgeon received green light to operate patients in Careggi with cadaveric tracheas, he changed his mind and insisted on using only plastic scaffolds instead. This radical departure from the approved protocol required a special review and new permit from Italian authorities. Yet when the Italian justice arrested him on suspicion of fraud and blackmail in 2012, Macchiarini just threw in the towel and moved his base entirely to Karolinska Institutet (KI) in Stockholm. Nanni Costa told me:
“We learned about PM’s transfer to Karolinska only from the newspapers”.
Careggi was practically kicked out of Biotrachea, the side project of cadaveric transplants abandoned completely and Macchiarini focused on plastic tracheas and more “healthy”, cancer-free patients, with the catastrophic results we know are all too well aware of. Yet at KI, he also operated with plastic tracheas two cancer patients, Beyene in July 2011 and Chris Lyles in November 2011. The latter had ACC cancer, just like Keziah and the Czech patient, yet he died just 2 months after the operation. Beyene had mucoepidermoid carcinoma (carcinoid tumour), an extremely slow-growing cancer with an excellent 5-year survival prognosis of 95% (Del Gaudio et al 2013). He only lived for 2 years after the operation, and suffered horribly during all this time.
Did Macchiarini really extend anyone’s life? We now know his plastic tracheas were a horrible death trap, but was at least one of his many cadaveric grafts useful in any way, or quite the opposite? How many people did he really transplant with cadaveric tracheas, and how many of them survived this miracle cure? Those directly involved keep silent: Careggi refused all communication with me, and UCLH deems me vexatious. Meanwhile, the London university hospital and Birchall are working to get their own derailed cadaveric trachea transplant trial back on tracks. For the greater good of the patients, presumably.

Donate!
If you are interested to support my work, you can leave here a small tip of $5. Or several of small tips, just increase the amount as you like (2x=€10; 5x=€25). Your generous patronage of my journalism will be most appreciated!
€5.00


Pingback: Boletim de Notícias, 6ª feira, 17/fev: Câmara aprova tratado do Aquífero Guarani | Direto da Ciência
Impressive. A REF2014 impact study (with broken link). What is the score?
LikeLike
We could assume all those transplants who led to death of the recipients were HUGE mistakes and lack of responsibility of the surgeons… The worse part is though, ALL involved institutions HIDE like criminals! That’s what we are as academics? A bunch of cowards that are afraid to face reality?
LikeLike
You have filled in the gaps rather convincingly, Leonid. I would applaud you, except much of what you are saying with regard to my daughter is incorrect. I won’t be giving you the information you have asked for. I have little respect for reporting that isn’t backed up by evidence. You are on dangerous ground.
LikeLike
Trace,
I completely understand your desire for privacy and I realize none of us truly know what your experience was. Aside from the troubling issues Leonid outlined here and in other posts, I’m personally concerned on general principles that patients and family members have adequate information before making decisions to participate in experimental interventions. Although this may not apply to your situation, I’m very concerned about what Chris Lyles and his family were told, especially about finances. According to various US new stories the family raised several hundred thousand dollars and mom took a mortgage on her (modest) home. One story reported how grateful Chris was that Paolo generously waived his fee at Karolinska, yet Paolo was on salary and would have no fee to waive. A Facebook post, now inaccessible, reported that when fundraising fell short of what Karolinska required, an anonymous Swedish couple stepped in to guarantee the remaining amount. While this didn’t mean Chris and his family wouldn’t have to pay the entire bill, it allegedly allowed the surgery to go forward as planned.
We subsequently learned in the KI report that as Chris was on the plane coming for surgery, Paolo coerced his department at KI to guarantee payment to the hospital. It seems the Swedish couple were fictional. Today, according to the KS report, the family still owes $ to KS. It might seem like the means justified the end but lies are unacceptable.
Long story short: sometimes the “how” can be as important as the “what” and it can be very difficult for families and others outside of research to understand the obligations researchers and institutions owe patients.
As you probably know, UCL commissioned an external review of regenerative medicine at the institution. I imagine somebody will contact you to ask about your experience. If not, you should consider contacting Stephen J Wigmore, University of Edinburgh (who is the designated leader) to share your experience. It’s important to have a human counterweight to medical records. A full understanding can only make things better for future patients.
I’m not happy writing this because it likely causes you sadness, and for this I apologize. I did however want to suggest there is at least as much concern for you as there is about the details of Paolo’s failings.
LikeLike
Pingback: Ciaran’s success story – For Better Science
Pingback: Macchiarini leaves Russia: federal grant denied and Kazan lab shut down – For Better Science
Pingback: Bioethicist Arthur Caplan calls for retraction of all Macchiarini papers – For Better Science
Pingback: Keziah’s deadly trachea transplant: UCL hospital’s secret – For Better Science
Pingback: Macchiarini’s trachea transplant patients: the full list – For Better Science
Pingback: How trachea transplanters tricked Andemariam Beyene to sacrifice himself for a Lancet paper – For Better Science
Pingback: Appeal to Italian Parliament for an investigation into trachea transplants in Florence by Paolo Macchiarini – For Better Science
Pingback: UCL fibs Parliament about trachea transplants – For Better Science
Pingback: Megagrant, the Russian docu-novel of Paolo Macchiarini – For Better Science