Bone marrow stem cells are magic, they can do everything. If you don’t believe it, you are simply a loser scientist and will never get funded.
Prior to his bombastic fall from grace, the celebrity surgeon and professor of regenerative medicine Paolo Macchiarini was considered a genius stem cell wizard and a miracle healer. He not only fully trusted bone marrow cells to generate any kind of tissue inside his patients, nay, he also published his results in highest profile journals like The Lancet (which, by standard academic definition, is proof enough that his theory and methods were valid). Macchiarini did not chase money, neither funding nor salary, it was chasing him. Even after media revealed mass patient deaths and gross inconsistency between Macchiarini’s published reports and the actual medical files of his patients, the Elsevier-run Lancet is reluctant to retract his papers.
Simply put, the faith in the force of the bone marrow stem cells is stronger than their science. These cells are often referred to as mesenchymal stem cells; basically they are those undifferentiated cells from the bone marrow which do not carry the established markers of hematopoietic (blood-generating) stem cells. What these “mesenchymal stem cells” are actually a mixture of, and which types of cells or tissues they are really able to differentiate into, is still a subject of an ongoing research. Unless you are a stem cell believer, that is, then you don’t bother with such details.
Bone marrow magic, from bench to bedside
At the turn of the century, the notion was established (largely through publications in certain very high profile journals), that these mesenchymal stem cells from the bone marrow were pluripotent, or multipotent at least. Meaning, they can practically generate any type of cells present in out body, just like the early embryonic stem cells of the blastocyst. How cool is this (i.e., if it were true)? One such discoverer was Catherine Verfaillie, who is now director of the Stem Cell Institute at the Catholic University (KU) Leuven in Belgium. Verfaillie published seminal papers in Nature (Jiang et al, 2002) and Blood (Reyes et al 2001). The latter publication was retracted for data manipulations; its first author was assigned all the blame. Verfaillie’s Nature paper was proven irreproducible and manipulated on top, but Nature’s faith in stem cell magic prevented a retraction: her paper was solely extensively “corrected”. Since then, the concept that bone marrow cells are anywhere near pluripotent was reluctantly discarded by stem cell scientists, who sometimes compensated this loss by (temporarily) finding pluripotency elsewhere, like the adipose tissue or spermatogonia. I am not sure Verfaillie herself still believes her old claims, she did not reply to my email.
At the University Clinic Düsseldorf, cardiology professor Bodo Strauer claimed to have cured heart attack patients with autologous bone marrow cell injections. The scandal of medical ethics and manipulated data was huge, yet even almost 10 years later, the Düsseldorf University finds itself unable to complete a misconduct investigation against their professor (see last part of my article here). Despite everything, the scientific literature is still teeming with papers proclaiming pluripotency of bone marrow cells. The fact that Macchiarini and his British collaborator, the UCL laryngologist Martin Birchall, chose to transfer some fishy basic science into dangerous clinical research by testing the regenerative capacity of bone marrow cells in trachea transplants on human patients, was only predictable and the next logical step.
In fact, Macchiarini was invited to perform his stem cell magic at the Swedish Karolinska Institutet (KI) by some of the most respected stem cell researchers in the world, namely Urban Lendahl and Ernest Arenas. They belonged to the 14 co-signers of the letter from 4th June 2010 (which I publish here) urging KI Rectorate to welcome Macchiarini’s regenerative medicine professorship and his clinical research with bone marrow stem cells. Other co-signers were the clinic head Li Felländer-Tsai and a number of otolaryngologists, including the department’s prefect Lars-Olaf Cardell and the hospital chief Richard Kuylenstierna.
Macchiarini’s method, apparently perfectly scientific to the KI throat surgeons and even world-renowned stem cell experts, was about extracting patient’s own bone marrow cells and to seed those onto a scaffold kept inside a plastic box called “bioreactor”, so they regenerate a transplantable trachea, including its mucosal epithelium, blood vessels, muscle tissue etc. Macchiarini developed this biologically somewhat incoherent approach together with Birchall at UCL. Their chosen scaffold was either a decellurised trachea from deceased donors (which bears dangers of immune rejection due to unavoidable tissue residues) or a plastic one, manufactured either at UCL by the nanotechnology professor Alexander Seifalian or by the US-based company Harvard Apparatus (now called Biostage). Either of these plastic tracheas proved a disaster. Because patients died after horrible suffering, the EU reversed its funding decision and terminated the cashflow for the major clinical trial Biotrachea, led by Macchiarini together with Birchall and Seifalian.
The blind faith into stem cell magic went at KI so far, that Macchiarini and his acolyte Philip Jungebluth (presently thoracic surgeon at University of Heidelberg, see my report here) were allowed to stuff some blood cells down their patient’s windpipe, in order to somehow achieve tissue regeneration. This “let’s just do it and see what happens” adventure was published in the journal Respiration as Jungebluth et al 2015, despite that the patient has been long dead at the time of manuscript submission. Only now did KI become worried about this “suspected scientific misconduct” and its “ambiguities” with “ethical approvals, among other things”. It became one of over a dozen of cases of misconduct where Macchiarini is now investigated by KI.
Now, after the Karolinska’s Ethics Chernobyl (as the surgeon Bo Risberg described it in his Open Letter), with Macchiarini sacked from his KI professorship and his EU funding terminated, did some realism and scepticism into the true regenerative capacities of bone marrow cells return? Far from it.
Say “stem cells!” for cash
The European Union, as well as other public funders, seem to be under impression that it was Macchiarini’s personal karma which prevented the perfectly capable bone marrow cells from regenerating tracheal tissue. Without Macchiarini, but with generous EU and British funding, his former close collaborator Birchall is about to start transplanting regenerated tracheas (as well as larynxes) into patients, possibly already this year.
As I reported earlier, Birchall’s TETRA Consortium, led by the UK-based company Videregen, and funded to 100% by the EU Horizon 2020 programme with near €7 Million, will be manufacturing tracheas in London and in Munich, and implant them into patients in UK, Austria, Italy and Poland. I set out to investigate how their current method is different to the one that Birchall developed together with Macchiarini. For this, I contacted the head of the TUMCells Centre at the Technical University Munich, Martin Hildebrandt. The Bavarian scientist was initially very eager to advertise his work to a journalist:
“We will manufacture the trachea transplants according to a technology transfer from London (UCL) as soon as the method is validated and a manufacturing permit is available. We will use the bone marrow blood of the designated recipient to colonise the decellurised windpipe of a cadaver donor”.
I asked whether they will also be using plastic scaffolds manufactured by Seifalian. Hildebrandt replied:
“we believe that artificial matrices do not vascularize well and hence do not function. Therefore we will use only decellurised tracheas of the deceased, which will formally serve as starting material for the production of our clinical trial samples (because this is a clinical trial within the meaning of the Medicines Act). More on this soon!”
However, nothing more was told. After some reminders, Hildebrandt politely referred me to Videregen’s CEO, Steve Bloor. Boor wrote to me on April 12th: “Thank you for your email enquiry. We will respond in due course”. Since then, all my follow-up emails were met with silence. No reply at all from any of the TETRA Consortium participants whom I attempted to contact. Neither was I given the empty patient consent forms and information brochures which I asked for, despite that these by definition can never be deemed confidential.
However, I received some information from the European Union. The EU spokesperson wrote to me:
“In the TETRA trial, natural, decellularised and re-seeded donor-derived trachea scaffolds would be used, whereas in other projects referred to, synthetic scaffolds were developed and used. Compared to other trials with donor-derived tracheas, the approach that would be used in TETRA is more sophisticated, by using two investigational medicinal products (IMPs) and supporting techniques (adding muscle or other tissue flaps to provide a vascular base for the new trachea). In addition, the decellularisation procedure that would be applied to donor trachea is more standardised and advanced compared to methods used in earlier trials”.
The bit about how Birchall’s current bone marrow stem cell approach to trachea repopulation is different from the highly debatable one that he and Macchiarini used to apply previously, is suspiciously missing from this EU spokesperson’s statement. This is strange, since I specifically asked about it. Either it is exactly the same method or it too secret to be disclosed to the public (though the same public is invited to participate in having this mysterious stem cell contraption implanted into their airway).
Otherwise, there are apparently two key advances to the previous Birchall/Macchiarini technology (which still cannot be disclosed in detail). These are the better decellurisation protocol for donor trachea, to avoid potentially lethal inflammatory response, and the use of tissue flaps to promote regeneration.
The stem cell party-poopers
I then asked some experts, of stem cell, regenerative medicine and tracheal surgery fields what they think of Birchall’s current technology.
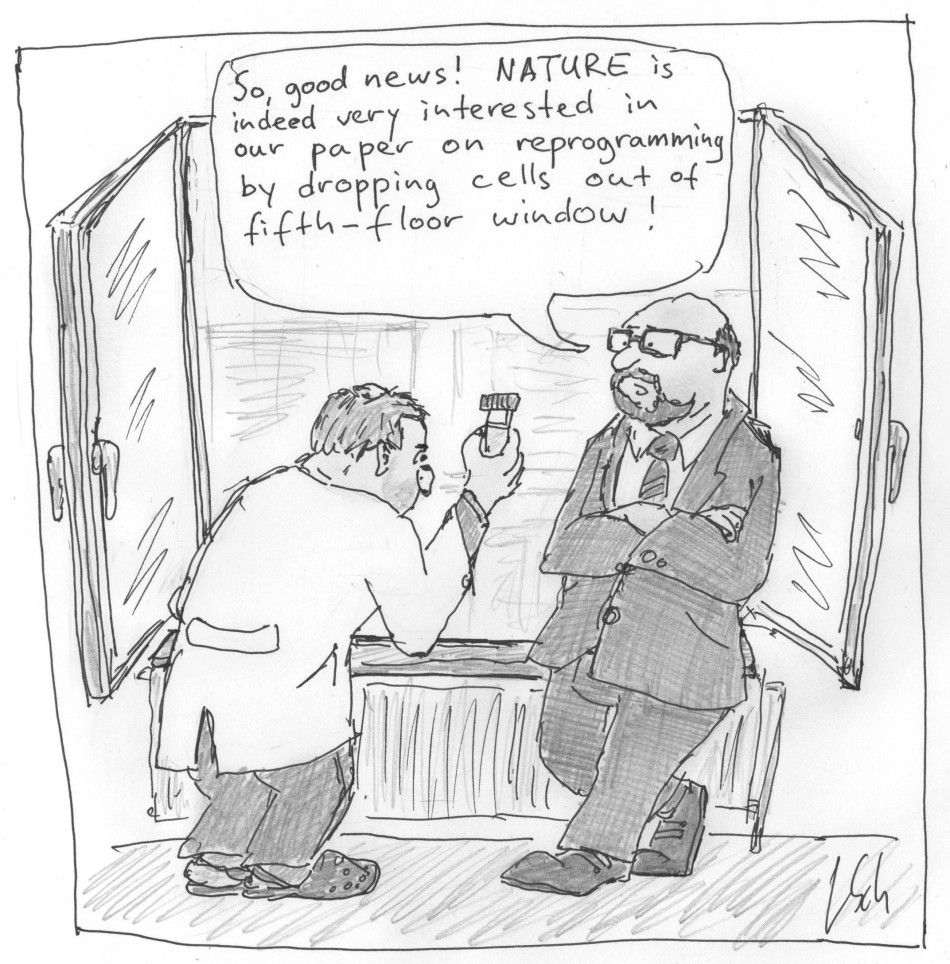
Kenneth Ka-Ho Lee is professor for stem cells and regeneration at the Chinese University of Hong Kong. He is well known as the first scientist to have experimentally disproved the notorious STAP fraud, where two 2014 Nature papers by Haruko Obokata and other researchers of the Japanese RIKEN institute and the Brigham&Women’s Hospital in Harvard claimed to magically transform cells into pluripotency by exposing them to an acidic environment. Lee was told by Nature that his work did not provide enough challenging evidence against STAP, so he published it in F1000Research (Tang et al, 2014). Soon however, Nature retracted both STAP papers (here and here) for excessive data manipulations, and the next year published a study by US-American and other elite western scientists disproving STAP (De Los Angeles et al 2015). So, what does Lee think of the advanced stem cell technology of the TETRA Consortium? Lee shared his views about the use of decellurised and bone-marrow regenerated human donor tracheas:
“This will not be an easy job as the trachea is makeup of a series of C-shaped hyaline cartilage rings. These cartilages will be difficult to completely decellularize. The use of autologous bone marrow stem cells is well tolerated and will not be immune rejected. However, do the bone marrow stem cells know that they have to differentiate into hyaline cartilage cells when seeded into the scaffold? Will inducing cytokines like BMPs be used to direct the differentiation of the bone marrow stem cells? Can the bone marrow stem cells fully migrate and penetrate the tolerate scaffold? Will the scaffold itself induce an immune response when transplanted into patients? Assuming a trachea implant could be produced in vitro, can the implant stimulate blood vessels from the host to grow into it – to keep it nourished and well oxygenated? Furthermore, the host blood vessels must grow fast enough and penetrate all regions of the trachea implant before part of this impact (deep tissues) start to die off. There are so many unanswered questions – will it not be better to try it out on a large animal first?”
Another expert I asked was Alexey Bersenev, stem cell researcher at the Yale School of Medicine. He describes himself as a “big proponent of clinical translation of tissue engineered organs”, yet insists on the “scientifically sound clinical translation”. Bersenev is also an active blogger of stem cell research, he recently specifically commented on the “Stem cell hype in clinical tissue engineering of hollow organs”, where he urged caution with Macchiarini’s and Birchall’s technology. Speaking to me about their trachea regeneration promises, Bersenev criticised the ”over-hyping ‘stem cell’ use”:
“Unfortunately, it is very typical for surgeons, who are “pushing the envelope” to stick “stem cell label” everywhere they can, without scientific rational. It is very much applicable to the use of total unfractioned freshly isolated bone marrow mononuclear cells (MNC) and adipose tissue-derived stromal vascular fractions. These populations of cells are very, very heterogeneous and contain a lot of other than “stem/ progenitor cells”, with significant therapeutic value. […]In bioengineered trachea, saturated with MNC, the evidence for therapeutic action of bone marrow stem cells is lacking. In my opinion, with lack of evidence, the only reason to use ‘stem cell’ term in grant application is to hype or exploit ‘sexy topic’ in order to get funding. It is not clear to me, if there is any value in using bone marrow MNC for saturation of bioengineered trachea construct. As far as I know, there are no studies, which compare trachea ‘with MNC’ vs. ‘without MNC’.”
Bersenev also pointed out that in regard to hollow organs bioengineering, he “was not able to find any good study on large animal models”. The two studies he pointed me towards (Clark et al 2016 and Wood et al 2014), in his view instead “demonstrated a lack of success and emphasized necessity of additional work”.
Update 26.04.2016, 23:30. Paul Knoepfler, professor for regenerative medicine at UC Davis and another prominent stem cell blogger, offered his insights as well (full comment below):
“Marrow cells and more specifically hematopoietic stem cells are not pluripotent. They are also generally not thought of as being particularly well-suited to form complex tissues […] Unfortunately we still keep seeing ‘magic’ invoked for what stem cells can do, but as promising as stem cells are, hype should be avoided and data should be king no matter what kind of stem cells one is focusing upon and no matter who is doing the work.”.
Also Graziella Pellegrini, professor for regenerative medicine at the University of Modena in Italy (and former Biotrachea participant) expressed her distrust into multipotency of bone marrow cells, in a comment below and over Twitter:
Finally, Macchiarini’s main critic Pierre Delaere, professor for respiratory surgery at KU Leuven (incidentally, same university where Verfaillie resides) offered his views as well. Delaere already summarised his criticisms from the surgeon’s perspective in his Open Letter on my site, now he gave these bullet point comment on the TETRA Consortium approach:
- “There is no evidence that the ‘decell-recell’ approach for tracheal regeneration can work.
- The previous ‘compassionate-use’ patients: no additional evidence: all of them are functioning with a stent or died shortly after the procedure.
- To make it all more acceptable: they intend to implant the tracheal construct in a muscle to add some blood supply: this make no sense and will not provide additional value for this non-existing regeneration concept”.
To sum up: a surgeon says the tissue flap is pointless and the stem cell experts are unconvinced what exactly Birchall and Co want the bone marrow cells to perform. Also, there seems to be little evidence of any success of their regenerative technology in animal models. Except of course, Birchall’s and Macchiarini’s own paper in this regard, namely Go et al 2009. One peculiar aspect is however: this proof-of-principle study on pigs was submitted for publication in May 2009, almost one year AFTER Macchiarini and Birchall operated their first human patient in Barcelona. According to Jungebluth’s own medical doctorate thesis (made under Macchiarini’s supervision), the preparation of donor trachea began in November 2007, the implantation into the patient Claudia Castillo occurred in June 2008. This worldwide-celebrated “scientific breakthrough” was published in The Lancet as Macchiarini et al, 2008. Regardless how trustworthy a Macchiarini paper is scientifically, here the therapy was apparently first tested on humans before proceeding into pigs. Now, the EU-funded TETRA Consortium seems inclined to do the same, on a much larger scale, in a clinical phase II trial (i.e., if they ever plan to test their methods on pigs as well).
Take the money and run?
Yet, after longish deliberations, EU announced to me something extraordinary. Despite the approved and theoretically available TETRA funding (officially listed as “from 2016-01-01 to 2019-12-31, ongoing project), the EU money will only be given to the Consortium members once they prove their method in the ongoing phase I trial, funded by a British funding agency. Here is the quote from the EU spokesperson I received:
“The TETRA phase II clinical trial is building on a prior phase I study, the INSPIRE trial. This trial was recently approved by the UK Medicines and Healthcare products Regulatory Agency, and is expected to start in the first half of 2016. It is not funded by the EU.
The TETRA project is currently in the preparatory phase, consisting largely of technology transfer between the project participants, training and accreditation of surgical procedures, and logistical preparations. In order to ensure the safety of patients, the Commission will conduct ethical assessments before the start of any clinical trial and on the basis of the preliminary safety evidence obtained from the INSPIRE phase 1 trial. The TETRA clinical trial may not start before a positive outcome is achieved in the phase I study, and all regulatory and ethics approvals have been obtained”.
It probably does not happen often that the funding for a phase 2 clinical trial was approved before phase 1 has even begun. Actually, the £2.4 Million funded INSPIRE trial was supposed to start in 2014 already, with 15 trachea-transplant receiving patients. Despite or because of the delay, the EU decided not to wait that long and simply allocated the €7 Mio for the follow-up TETRA phase 2 trial in advance.
Chances are, if the results of INSPIRE clinical trial are unconvincing, the EU might terminate their funding to TETRA. It will be another major setback to Birchall and his colleague Mark Lowdell, Director of Cellular Therapy at UCL and Royal Free Hospital, after the EU killed the Biotrachea programme, and after the University of California Davis cancelled the $4.4 Million collaboration project with the UCL doctors on stem cell-driven airway transplants due to “logistical difficulties of intercontinental collaboration”. Logistics seem to be a tricky issue in regenerative medicine.
Birchall however still has plenty of regenerative work ahead. He currently started recruiting patients for his RegenVox trial, where they will be receiving a decellurised larynx transplant, seeded with patients’ own bone marrow cells. The trial is funded with almost £3 Million by the British MRC, and was supposed to begin already in 2013. Now, in mid-2016, Birchall and his team are good to go.
Also with RegenVox, the Belgian throat surgeon Delaere advises patients to caution:
“The people who have written and approved this protocol are completely unaware of reconstructive surgical techniques and wound healing mechanisms[…]. From a theoretical point of view: hilarious how they want to create a cartilaginous scaffold, wrap it into a muscle and hope that this construct can do something for laryngotracheal repair[…]. Even in case they would succeed in repopulation and create something like a cartilaginous framework, it would be useless because it has no mucosal lining (and will never accept a lining)”.
Delaere finally points to his group’s own publication on a reconstruction technique of extended laryngeal defects with vascularized tracheal autotransplants (Loos et al 2016). The method was developed by Delaere and colleagues already 10 years ago, yet Birchall seems to have overlooked it. At least he never acknowledged its existence in his publications.
The great potential
All considered, bone marrow cells do not seem to be doing much when seeded on trachea scaffold, even when locked up in a bioreactor and sternly instructed to regenerate tracheal tissue by qualified elite clinical scientists at UCL or Karolinska. When they find themselves inside this doctor-duped patient’s airway, the bone marrow cells most likely just die. Their application however bears a certain risk of microbial infection or inflammation. But this residual risk to individual patients is surely utterly negligible compared to the tremendous and reproducible effect which the bone marrow stem cells have robustly demonstrated on opening the funders’ coffers and publishing in high impact journals. And isn’t this what most of academic research is actually about?
The author wishes to thank Elizabeth Woeckner for continuous sharing of valuable information
Update 12.05.2016. My attempts to procure patient information brochures and empty consent forms for the Birchall-run trachea transplant trials prove rather difficult. These documents concern the four-patients-based phase 1 INSPIRE trial happening or recruiting right now, as well as the upcoming phase 2 trial, run by TETRA consortium with EU funding. Videregen and the TETRA participants refused to share these public documents with me, I therefore submitted FOIA inquiries to UCL on April 22nd. Alex Daybank, UCL officer for Data Protection & FOI stated on May 10th:
“I am informed that The TETRA project is in the technology transfer phase in preparation for the clinical trial. Clinical documentation has not yet been finalised. When completed, the clinical protocol and associated documentation will be submitted to national Competent Authorities and national ethics committees for approval before the trial is authorised to commence in compliance with Good Clinical Practice in accordance with EU Clinical Trial Directives“.
After I pointed out that my FOIA inquiry to the phase 1 INSPIRE was overlooked, Daybank promised a reply by May 23rd. Today I received a note from Theodora Brocke-Afful,
UCLH Records Supervisor/FOIA, that I “should receive a response by 9 June 2016”. I was also warned that my request may be denied if it falls under one of “23 exemptions”. So much delay for brochures usually lying about in doctor’s waiting room and immediately available to any potential patient.

I agree that the story of magic mesenchymal stem cells, doing everything, has nothing to do with science and many patients had problem for that, however this approach was never included in EU project BIOTRACHEA, where epithelial cells were included and were supposed to originate from epithelial biopsy: not from mesenchymal cells.
I noted that the Italian group in the TETRA consortium, comes from Brescia, where Stamina story had the main headquarter. Why people in Brescia so strongly believe in multi potency of mesenchymal stem cells?
LikeLike
Actually, M. REyes is a coauthor (#7) in Jiang et al (Nature, 2002).
LikeLike
Thanks, corrected!
LikeLike
Marrow cells and more specifically hematopoietic stem cells are not pluripotent. They are also generally not thought of as being particularly well-suited to form complex tissues. One would have a better chance in the kind of applications discussed here by using pluripotent stem cells such as IPS cells, but even there it’s a tough road to prove safety and efficacy.
Another relevant context to bring in here is that there’s a big push under way in the stem cell field globally and in the US to allow introduction of experimental adult stem cells, primarily MSCs, into patients based upon far less data than is now required. For instance, some big wigs support the idea of skipping Phase III trials and having conditional approval of stem cell drugs that are not well-vetted experimentally. Some in this group also approve of the idea of charging patients to be in such trials. I oppose these changes, which I think are risky both to patients and the field, and I’ve blogged about my concerns over at the Niche. The kind of bad outcomes and problems described in this post point strongly to reasons for caution in pursuing such regulatory changes that would weaken oversight and data requirements. Japan has already implemented weaker regulatory oversight of as yet still experimental regenerative medicine and stem cell “treatments” and there are concerns that patients could well be harmed by this “rush to treat”.
It may not be a perfect analogy, but pushing for less oversight of experimental stem cell treatments is kind of akin to saying that there should be far less review of submitted grants and manuscripts (maybe 1 reviewer instead of 2-4) on stem cells because the review process is too slow and is impeding going from bench to bedside.
Unfortunately we still keep seeing “magic” invoked for what stem cells can do, but as promising as stem cells are, hype should be avoided and data should be king no matter what kind of stem cells one is focusing upon and no matter who is doing the work.
LikeLike
If there really is any use of induced autologous stemcells it will take long time before anyone will be convinced of it. That is, after these charlatans have killed enough people to make it obvious what they are doing, its not enough with some 6+ victims apparently.
LikeLike
Please note this from Mark Lowell’s previous foray into clinical trials. Dodgy over-claim for a commercial venture in which he had an interest had to be sorted by UCL clinical governance procedure.
The complexity of Good Clinical Practice compliance was underestimated and led to failures requiring retrospective independent data review. The lessons learned are an important aspect of this report.
LikeLike
Thank you Ms Henrietta 🙂 http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0123416
Failure to appreciate the complexity of Good Manufacturing Practice and well as GCP may go some ways to explain the oddities in the INSPIRE and RegenVOX trials.
According to the 2014 research impact report by Birchall, they developed GMP-compliant preparation of decell-recell cadaveric tracheas: http://www.circare.org/info/pm/ucl-impact-2014.pdf
Further, he writes that
“We found that we were able to substantially accelerate the process of decellularisation by using a variable pressure based method allowing for removal of all nuclear material within the overlaying muscle and cartilage over a seven-day period [4]. The technique preserved anatomy, including critically the vocal cords, and biomechanical strength including the structural integrity of the collagen, in a quarter of the time taken by conventional protocols. Again, this method was successfully field-tested in the production of a robust, easily recellularised, tracheal graft for a second child.”
And finally
“We generated flexible sheets of mucosa from autologous epithelial progenitor cells for rapid functionalisation of hollow organs as well as GMP transport and storage processes.”
It seems however the variable pressure decell protocol has been abandoned in favor of a negative pressure protocol, patented by Videregen, according to this press release: http://www.videregen.com/clinical-trial-for-replacement-trachea-technology-to-start-next-year/
Patent: http://www.google.com/patents/WO2014202958A1?cl=en
Publication: http://onlinelibrary.wiley.com/doi/10.1002/term.1979/full
(would Tahera Ansari like to disclose the patent application?)
Decellularization will be done by NHS Blood and Transplant, not UCL or Royal Free. GMP problems? Perhaps.
The most striking item is the change in the number of subjects to be enrolled in the INSPIRE trial. In the 2014 impact statement, 15 subjects were to be enrolled, yet in the Nov. 2015 Videregen press release, 4 (four) subjects will be enrolled in the trial. Right about now somebody ought to throw the bullshit flag. While ethical considerations frequently limit the number of subjects in phase 1 trials, INSPIRE is unique in that funding is already awarded for a phase 2 trial. Four subjects will not provide enough data to decide whether exposing 48 more subjects to risk of permanent harm or death in phase 2 is appropriate.
You have to wonder if inexperience in GMP wasted funds to the point that the trial can only afford to enroll 4 subjects. Are there other answers?
People need to start asking questions about the phase 2 award – how the heck can you get funding without data? Must have been a damn short review meeting.
As for RegenVOX, the sheets of epithelial progenitor cells would indeed be helpful to line the decell larynges and in fact Birchall and co. published a paper on this: https://www.ncbi.nlm.nih.gov/pubmed/26840431
So it’s baffling that at the end of 2014 the RegenVOX trial protocol was revised to eliminate seeding of the graft with epithelial cells in favor of a split thickness skin graft: https://clinicaltrials.gov/archive/NCT01977911/2014_12_07/changes
With respect to decell cadaveric trachea transplants, Birchall has one child who died after 23 days from massive bleeding in the chest and the Irish boy with a stent. Macchiarini had at least 8 patients (2 in Barcelona, 5 at Careggi and 1 in Moscow), all of whom are either dead or failures, this latter according to the director of the Italian National Transplant Center: http://corrierefiorentino.corriere.it/firenze/notizie/cronaca/16_febbraio_08/macchiarini-verdict-from-rome-f4922444-ce73-11e5-84b6-e3afc18b58d6.shtml
See also this article in the Corriere Fiorentino: http://tinyurl.com/hj92t9o
LikeLike
The complexity of Good Clinical Practice compliance was underestimated and led to failures requiring retrospective independent data review. The lessons learned are an important aspect of this report.
This from Mark Lowell’s previous foray into clinical trials. Poor practise required UCL clinical governance to step in before the paper made a hyped claim for a company with which Lowell was associated.
LikeLike
Anna Hörnlund, Chief Legal Counsel at the Swedish Research Council, stated, on April 30, 2016, in the Lancet:
“On Jan 1, 2004, a law came into force in Sweden concerning the ethical review of research conducted in human beings. This law covers research conducted in living human beings, on human cadavers, and on biological material from human beings, and the handling of sensitive personal information. The Swedish Research Council considers Paolo Macchiarini’s activities1 to be research conducted in human beings.
When research is conducted in human beings, the principal investigator (defined as the state agency or the physical or legal entity under whose organisation the research will be conducted) is obligated by Swedish law to apply for an ethical review. The application must be submitted to one of six regional ethical review boards. These review boards are individual public authorities. Neither Macchiarini, nor the Karolinska Institutet, has submitted such an application.”
http://www.thelancet.com/journals/lancet/article/PIIS0140-6736%2816%2930320-8/fulltext
So, jail time and retraction(s) eminent?
LikeLike
Pingback: Cells Weekly – May 1, 2016
There is too much money buried in MSCs-related biotechs. There will always be a lot of pressure on government agencies to look the other way. Besides, it’s not only doctors that push the envelope in situations like these; engineers, such as the ones designing the plastic windpipes, also help to create this expectation bubble around MSC. They just use MSC as the carrot to get funding for their own material/biomaterial technologies. Since everyone knows eachother, it is very easy to maintain the artificial hype in the different journals of the fied. But one day the bubble will burst. And the sooner, the better.
Having said that, I do believe MSCs (or whatever they may be) hold great regenerative potential, maybe not just in the form of a multipotent cell source for differentiation.
LikeLike
That’s quite an interview with Macchiarini, revealing, and brutal:
http://www.svtplay.se/video/8150958/aktuellt/aktuellt-4-maj-21-00
The interviewer asks “Are you a pathological liar?”
Right near the end of his interview, Macchiarini states:
“The scientific articles, as far as I understand, I was cleared from all the scientific misconduct accusations.”
LikeLike
Any thoughts as to the claims from Sergei Paylian of Bioquark that he can reconstruct the brains of brain-dead bodies in situ using stem cells (created by restoring nerve cells to pluripotency with his patented electroporation / xenopus oocyte technology), without any of the massive neural migration and remodelling that normally occurs in the development of a brain? It sounds like total crankstuff to me.
LikeLike
Goodness gracious. Is everyone mad out there?? http://www.telegraph.co.uk/science/2016/05/03/dead-could-be-brought-back-to-life-in-groundbreaking-project/
LikeLike
Paylian’s publications are all through lower-echelon predatory publishers like Bioaccent (whose spam takes the unusual approach of stressing that they have no impact factor and therefore no standards).
Click to access cancer-sciences08.pdf
His patent for creating pluripotent stemcells (by incubating the cell-line of choice within or beside xenopus oocytes, plus “co-electroporation”) is 5 years old.
http://patents.justia.com/patent/20110143415
Ever since then he has been claiming that this technology can rebuild any organ. So why start with brains? Why nothing else in the meantime?
I noticed that the permission he’d been granted for his “proof-of-concept” trial, at an Indian hospital, quickly morphed in the UK media into “approved by US health watchdogs”. Was that the Telegraph’s own fabrication, before they edited out the reference to “an Institutional Review Board at the National Institutes of Health in the US”? Or did they simply pass on a lie from the company?
LikeLike
No, wait, it gets better — Bioquark are running this project through the US NIH, with official NIH ethical blessing:
https://clinicaltrials.gov/ct2/show/NCT02742857
So why Sarah Knapton revised the Telegraph story is anyone’s guess, and I owe both her and Bioquark an apology.
LikeLike
Registration on Clinicaltrials.gov has nothing to do with NIH approval. Registration is self-serve and open to anyone. The database is now under the authority of FDA and while this means relatively timely attention to funky registrations of trials testing products under FDA jurisdiction, FDA can’t do anything about other trials. I believe but cannot confirm that FDA reports problematic registration to the competent authorities.
NIH IRBs review trials conducted at NIH by NIH employees with the exception of the NCI IRB which offers cooperative review of oncology trials sponsored by NCI.
If you go to the end of a trial registration there are fields for source of funding/sponsorship and health authority.
The Telegraph erroneously reported an “approach” (typo for approval?) by an NIH IRB & sane people complained to NIH.
LikeLike
Thanks!
The Clinical Trial listing at the Indian registry is slightly more informative:
http://ctri.nic.in/Clinicaltrials/pmaindet2.php?trialid=14796
I learned that one of the multimodalities of Woo to be administered to the brain-dead bodies includes “Bioquantine”, which is squeezed out from amphibian egg-cells after “activating” them and supposedly communicates their pluripotent capacity to human cells. It will be injected directly into spinal fluid.
http://www.google.com/patents/WO2014018663A1?cl=en
In the Indian version, Dr Himanshu Bansal is the Principal Investigator (not just a partner). He runs the hospital for the indigent where he intends to recruit patients.
LikeLike
Paul Knoepfler blogs about this outrageous and deeply unethical pseudoscience: http://www.ipscell.com/2016/05/not-zombies-but-bringing-back-the-dead-with-stem-cells-lasers/
LikeLiked by 1 person
Paul notes that the intended injections of stem cells and frog-egg squeezings “would be done in combination with laser stimulation of the brain. I need to learn more, but how exactly could lasers affect the brain positively?”
— Not to forget the fourth component of the protocol, laser stimulation of the median nerve (in the wrist). A while ago, electric stimulation of the median nerve was in vogue as a way of repairing brain damage, but the quacks moved on from electrodes to lasers as being more science-y. I think it’s a chiropractice thing.
The reason why Dr Bansal is offering this odd and unexplained combination of “modalities” is simply that his Revita Life Sciences company already has the lasers lying there in the clinic:
http://revitalife.co.in/low-level-laser-stimulation/
He also offers hyperbaric oxygen, naturopathy, Ayurveda and healing electromagnetic pulses. I can practically hear the spooky theremin music playing in the background.
LikeLiked by 1 person
Sarah Knapton at the Torygraph is evidently happy with her role of mouthpiece for Revita’s press releases:
http://www.telegraph.co.uk/science/2016/05/09/trial-starts-to-bring-dead-27-year-old-car-crash-victim-back-to/
LikeLike
Pingback: Macchiarini’s patients, the real situation – For Better Science
Pingback: EU threatens to terminate TETRA Consortium funding for phase 2 trachea transplant trial – For Better Science
Pingback: Brexiting out of EU research and patient rights – For Better Science
Pingback: Regenerating in Hannover, Part 2: Axel Haverich’s “growing” heart valves – For Better Science
Pingback: Does ERC help cheaters pay protection money? – For Better Science
Pingback: Growing hearts in Hannover: a job opening – For Better Science
Pingback: How UCL throat surgeon Martin Birchall misleads patients and tricks public funders – For Better Science
Pingback: Macchiarini investigations outcome: the Karolinska Institutet – For Better Science