“Doctor, please, some more of these…” -The Rolling Stones (1966)
Antidepressants, specifically those of the Prozac family are the new game-changer miracle drugs of choice in this pandemic. The pattern is very similar to hydroxychloroquine and other repurposed medicinal products: scientists take some medicine which has nothing to do with virology, infectious diseases or even inflammation as the new COVID-19-crusher, simply because this is the drug they themselves have been working with all their lives. Other scientists jump on the bandwagon, run retrospective clinical analyses and in vitro tests, and seem to confirm the breakthrough results.
Science has spoken, a hype is created, with stormed pharmacies and emergency use authorisations by either desperate or criminal governments because people are dying. Much later, large randomized controlled clinical trials with thousands of patients participating and many millions of euros and dollars invested prove the new COVID-19 drug never actually worked. The world moves on to the next repurposed miracle cure. Think of Didier Raoult and his with obsession with the malaria drug chloroquine, and what that ended in.
This might be now happening with fluoxetine (marketed as Prozac) and other members of this Selective Serotonin Reuptake Inhibitor (SSRI) antidepressant family. Or maybe psychiatrists did save the humanity after all?
Most recently, a German scientist announced in all national media a cure for COVID-19. Virology professor Jochen Bodem from the University of Würzburg found the drug to kill the SARS-CoV2 virus: fluoxetine. The peer-reviewed paper was published this month, March 2021:
Melissa Zimniak, Luisa Kirschner, Helen Hilpert, Nina Geiger, Olga Danov, Heike Oberwinkler, Maria Steinke, Katherina Sewald, Jürgen Seibel & Jochen Bodem The serotonin reuptake inhibitor Fluoxetine inhibits SARS-CoV-2 in human lung tissue Scientific Reports (2021) doi: 10.1038/s41598-021-85049-0
The study is based on a bioRxiv preprint dating back to June 2020, with less authors. It was supported by the pharma industry: “[Bodem] has been funded by Novartis“. The authors wrote:
“To circumvent time-consuming clinical trials, testing whether existing drugs are effective inhibitors of SARS-CoV-2, has led to the discovery of Remdesivir. We decided to follow this path and screened approved medications “off-label” against SARS-CoV-2. In these screenings, Fluoxetine inhibited SARS-CoV-2 at a concentration of 0.8µg/ml significantly, and the EC50 was determined with 2.5ng/ml. Fluoxetine is a racemate consisting of both stereoisomers, while the S-form is the dominant serotonin reuptake inhibitor. We found that both isomers show similar activity on the virus. Fluoxetine treatment resulted in a decrease in viral protein expression. Furthermore, Fluoxetine inhibited neither Rabies virus, human respiratory syncytial virus replication nor the Human Herpesvirus 8 or Herpes simplex virus type 1 gene expression, indicating that it acts virus-specific. We see the role of Fluoxetine in the early treatment of SARS-CoV-2 infected patients of risk groups.“
Prozac, the antidepressant, is miraculously specific for the coronavirus, if this is not proof of intelligent design, I give up.
Btw, the same University of Würzburg used to celebrate their disastrously failed trachea transplants years ago, maybe they should be more careful before touting in vitro studies. Everything works to kill the virus in a dish, even licorice or artemisia extracts, as other German scientists proved.
Wait, didn’t I just tell you the cure was discovered by some psychiatrists repurposing their favourite drugs? Prof Bodem is a virologist after all, not a psychiatrist, who according to his publications stumbled upon fluoxetine all by himself, using nothing but his mighty scholarly brain to screen all existing medicines before arriving on the serotonin uptake inhibitors!
Maybe. Or maybe Professor Bodem read about news reporting from France and USA in spring 2020, about clinical studies initiated by psychiatrists.
Indeed, France is where the best magic cures for COVID-19 come from (not just Raoult’s chloroquine, remember the €5 million-secret of the rectal suppository from Lille?). The Parisian psychiatrist Nicolas Hoertel decided some day in spring 2020 that an antidepressant from the same SSRI family as Prozac, namely fluvoxamine (aka Luvox), must help against COVID-19, because of the buzzword “cytokine storm”.
So Hoertel did a retrospective clinical study on patient records in French hospitals.
Nicolas Hoertel, Marina Sánchez Rico, Raphaël Vernet, Nathanaël Beeker, Anne-Sophie Jannot, Antoine Neuraz, Elisa Salamanca, Nicolas Paris, Christel Daniel, Alexandre Gramfort, Guillaume Lemaitre, Mélodie Bernaux, Ali Bellamine, Cédric Lemogne, Guillaume Airagnes, Anita Burgun, Frédéric Limosin Association between antidepressant use and reduced risk of intubation or death in hospitalized patients with COVID-19: results from an observational study. Molecular Psychiatry (2021) DOI: 10.1038/s41380-021-01021-4
It was based on a bioRxiv preprint from August 2020, which declared:
“Participants 7,345 adults hospitalized with COVID-19 between 24 January and 1 April 2020, including 460 patients (6.3%) who received an antidepressant during the visit.”
Hoerter (who declared “personal fees and non-financial support” from the pharma company Lundbeck) and his psychiatry colleagues discovered:
“Specifically, exposures to escitalopram, fluoxetine, and venlafaxine were significantly associated with lower risk of intubation or death (all p<0.05).“
Just look at these results:
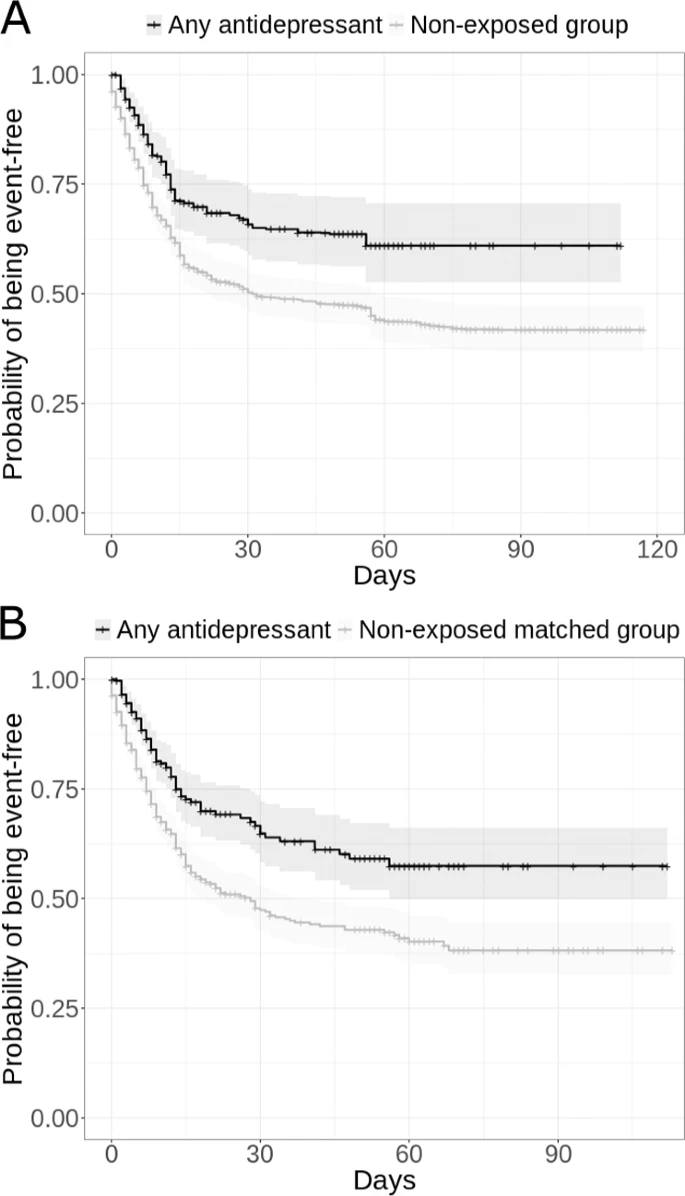
In Hoertel’s analysis, not just Prozac, any antidepressant, SSRI or not, worked like a charm.
In United States, the psychiatry professors Angela Reiersen and Eric Lenze of the Washington University had the same idea with SSRI antidepressants. They in turn arrived at their drug by reading the fluvoxamine research on sepsis from February 2019, by Alban Gaultier and his PhD student Dorian Rosen at the University of Virginia. The study (Rosen et al Science Transl Medicine 2019) claimed that fluvoxamine “protects mice from lethal septic shock and dampens the inflammatory response in human blood leukocytes“.
Lenze and Reiersen then set up a clinical trial (NCT04342663) on 152 patients which recruited from 10 April 2020 till 5 August 2020, with a 15 day follow-up. The results were published in the elite journal JAMA in November 2020, Lenze declared receiving grants and consulting fees from Janssen and other pharma companies:
Eric J. Lenze, Caline Mattar, Charles F. Zorumski, Angela Stevens, Julie Schweiger, Ginger E. Nicol, J. Philip Miller, Lei Yang, Michael Yingling, Michael S. Avidan, Angela M. Reiersen Fluvoxamine vs Placebo and Clinical Deterioration in Outpatients With Symptomatic COVID-19: A Randomized Clinical Trial JAMA (2020) doi: 10.1001/jama.2020.22760
It was however just 115 patients who completed the 15 day assessment after treatment, yet also the 37 who didn’t complete were still included in the final analysis:
“Of 152 patients who were randomized (mean [SD] age, 46 [13] years; 109 [72%] women), 115 (76%) completed the trial. Clinical deterioration occurred in 0 of 80 patients in the fluvoxamine group and in 6 of 72 patients in the placebo group (absolute difference, 8.7% [95% CI, 1.8%-16.4%] from survival analysis; log-rank P = .009). The fluvoxamine group had 1 serious adverse event and 11 other adverse events, whereas the placebo group had 6 serious adverse events and 12 other adverse events.“

A very small study, as the authors themselves admit. The University of Washington scientists now seek to recruit 1,100 participants for a telemedicine clinical trial with fluvoxamine called Stop COVID, which, is funded by the Silicon Valley entrepreneur Steve Kirsch with half a million dollars, via his CETF foundation. There is also a Canadian arm at McGill University:
It was also Kirsch who funded the previous 152 patients study, and whose idea it was to publish the results in JAMA.
On TV, the JAMA results were celebrated as nothing short of miracle, but elsewhere the authors admitted the data was impressive yet somewhat inconclusive:
“among 80 patients took fluvoxamine, none developed low oxygen levels. Of 72 patients who took a placebo — a pill that does nothing – six developed low oxygen levels.
One of the patients who took fluvoxamine was hospitalized with dehydration. Four of the patients who took a placebo were hospitalized with Covid-19 related symptoms, and one ended up in the intensive care unit on a ventilator. The researchers did not look to see whether the hospitalization differences between the two groups was statistically significant.“
I don’t believe Lenze and Reiersen didn’t look. Their own trial registration included hospitalization as secondary endpoint.
The drug is now being prescribed to COVID-19 patients off-label in USA, for example by the medical entrepreneur and “race track doctor” David Seftel as told recently on US television.
“Sixty-Five patients elected to take fluvoxamine. Forty-eight declined. 12.5% of all those who refused fluvoxamine ended up hospitalized and one died. In the group that did take fluvoxamine, none of them were hospitalized. Once again – none of the covid patients taking fluvoxamine deteriorated.”
Just before the TV event, Seftel published these results together with David Boulware, infectious disease professor at University of Minnesota. Expert science journalists described this as “real-world study“, which probably means its results are more real than anything done in clinical trials.
David Seftel, David R Boulware Prospective Cohort of Fluvoxamine for Early Treatment of Coronavirus Disease 19 Open Forum Infectious Diseases (2021) doi: 10.1093/ofid/ofab050
“Incidence of hospitalization was 0% (0 of 65) with fluvoxamine and 12.5% (6 of 48) with observation alone. At 14 days, residual symptoms persisted in 0% (0 of 65) with fluvoxamine and 60% (29 of 48) with observation.“
Truly a miracle, call Stockholm and the Vatican.
Presently, the institutional website of Lenze’s “Healthy Mind” lab informs patients:
“fluvoxamine is a safe drug when prescribed correctly (see below), and many doctors are interested in prescribing it now. We cannot advise for or against it. Still, for those using fluvoxamine as a potential early treatment for COVID-19 , we recommend starting it at 100mg twice daily and then reducing it to 50mg if there are problematic side effects (about 25% of people develop nausea, which is mild though annoying for some). We do not think that increasing the dose to 300mg is necessary for its effect. We understand that some physicians are using a lower dose of 50mg twice daily to try to minimize nausea that can occur.”
To me, this sounds like some very detailed medical advice.
Also in April 2020, another US psychiatrist, Cheryl McCullumsmith, of the University of Toledo (in Ohio, not in Spain) decided that Prozac must be the cure for COVID-19. Basically, the university asked its scientists to do something about the pandemic as it arrived in USA, and the Chair of Psychiatry McCullumsmith chose fluoxetine aka Prozac, apparently because this is what psychiatrists choose in such situations. Her logic was:
““Fluoxetine has extraordinarily strong evidence in its action as a blocker of IL-6 and cytokine storms in both animal models of infection and in human illness such as rheumatoid arthritis and others,” McCullumsmith said. “This project aims to prevent serious outcomes such as hospitalization, respiratory failure and death in people when they are first infected with COVID-19. The goal is to use an existing drug in a new way to prevent serious complications of COVID-19 during the time it will take scientists to develop more lasting solutions, such as vaccines and antiviral treatments.”
That “cytokine storm” of uncontrolled inflammation again, which back in 2020 (and even now) was the general concept to explain COVID-19 and to somehow justify the use of chloroquine, ivermectin, colchicine and literally everything else.
A clinical trial with 2,000 COVID-19 patients was announced by the University of Toledo, also in April 2020. But McCullumsmith’s project hasn’t delivered anything so far, or it would have been mentioned in the recent press release from February 2021 where she congratulated Hoertel on his paper and again spoke of the “cytokine storm”.
I wonder if you noticed the confusion. The French and the Americans say Prozac cures COVID-19 by preventing inflammation (“cytokine storm”), the Germans say it works by direct inhibition of the viral activity (Bodem et al: “Fluoxetine presumably targets the virus directly“), as tested in vitro (where the immune system obviously is not part of the experimental setup). So like with chloroquine before, we scratch our heads and ask: which one is it? Immunomodulation or antiviral mechanism?
It seems the Germans do see Prozac and other antidepressives as direct antiviral drugs, here a study from the University of Münster, published in September 2020:
Sebastian Schloer, Linda Brunotte, Jonas Goretzko, Angeles Mecate-Zambrano, Nadia Korthals, Volker Gerke, Stephan Ludwig, Ursula Rescher Targeting the endolysosomal host-SARS-CoV-2 interface by clinically licensed functional inhibitors of acid sphingomyelinase (FIASMA) including the antidepressant fluoxetine Emerging Microbes & Infections (2020) doi: 10.1080/22221751.2020.1829082
Ursula Rescher is professor for host-pathogen interaction who specialises in endosomes, and her study with “No potential conflict of interest” postulated:
“We find that fluoxetine, a widely used antidepressant and a functional inhibitor of acid sphingomyelinase (FIASMA), efficiently inhibited the entry and propagation of SARS-CoV-2 in the cell culture model without cytotoxic effects and also exerted potent antiviral activity against two currently circulating influenza A virus subtypes, an effect which was also observed upon treatment with the FIASMAs amiodarone and imipramine. Mechanistically, fluoxetine induced both impaired endolysosomal acidification and the accumulation of cholesterol within the endosomes.“
Here, it’s endosomes and cholesterol. Days after, another German in vitro study claiming similar, but not identical molecular mechanisms of SARS-CoV2 inhibition appeared:
Alexander Carpinteiro, Michael J. Edwards, Markus Hoffmann, Georg Kochs, Barbara Gripp, Sebastian Weigang, Constantin Adams, Elisa Carpinteiro, Anne Gulbins, Simone Keitsch, Carolin Sehl, Matthias Soddemann, Barbara Wilker, Markus Kamler, Thomas Bertsch, Karl S. Lang, Sameer Patel, Gregory C. Wilson, Silke Walter, Hartmut Hengel, Stefan Pöhlmann, Philipp A. Lang, Johannes Kornhuber, Katrin Anne Becker, Syed A. Ahmad, Klaus Fassbender, Erich Gulbins Pharmacological Inhibition of Acid Sphingomyelinase Prevents Uptake of SARS-CoV-2 by Epithelial Cells Cell reports. Medicine (2020) doi: 10.1016/j.xcrm.2020.100142
The authors (who all “declare no competing financial interests“) gave some trial participants a nasal spray with a different antidepressive drug, Amitriptyline, picked their noses for some epithelial cells and infected those in vitro with the coronavirus. Thing is, amitriptyline is not of the SSRI family and works via a different molecular mechanism than fluoxetine. And yet it worked, just like Hoertel predicted:
“Treating volunteers with a low dose of amitriptyline prevents infection of freshly isolated nasal epithelial cells with pp-VSV-SARS-CoV-2 spike. The data justify clinical studies investigating whether amitriptyline, a safe drug used clinically for almost 60 years, or other antidepressants that functionally block acid sphingomyelinase prevent SARS-CoV-2 infection.“
The cancer research professor Erich Gulbins of University of Duisburg-Essen postulated a specific antiviral mechanism which Bodem didn’t have, but which matches that of Rescher’s: the antidepressives must work via the sphingomyelinase enzyme, which reduces ceramide production and thus prevents the coronavirus from entering the cell. Or so Gulbins’ idea goes. Btw, small world: Gulbins is also Editor-in-Chief of a journal which has been overrun by paper mill fabrications, as uncovered by Smut Clyde and Tiger BB8. I quoted him in my related reporting.
Moving on. Finnish scientists (“no competing interest“) also say it doesn’t matter which antidepressive drug you use, they all prevent virus replication. The preprint was published just this week, on 23 March 2021:
Senem Merve Fred, Suvi Kuivanen, Hasan Ugurlu, Plinio Cabrera Casarotto, Lev Levanov, Kalle Saksela, Olli Vapalahti, Eero Castrén Antidepressant and antipsychotic drugs reduce viral infection by SARS-CoV-2 and fluoxetine show antiviral activity against the novel variants in vitro bioRxiv (2021) doi: 10.1101/2021.03.22.436379
Basically, almost anything goes, but Prozac (fluoxetine) is the best:
“Several clinically used antidepressants, including fluoxetine, citalopram, reboxetine, imipramine, as well as antipsychotic compounds chlorpromazine, flupenthixol, and pimozide inhibited the infection by pseudotyped viruses with minimal effects on cell viability. The antiviral action of several of these drugs was verified in Calu-1 cells against the (B.1) lineage of SARS-CoV-2. By contrast, the anticonvulsant carbamazepine, and novel antidepressants ketamine and its derivatives as well as MAO and phosphodiesterase inhibitors phenelzine and rolipram, respectively, showed no activity in the pseudovirus model. Furthermore, fluoxetine remained effective against pseudo viruses with N501Y, K417N, and E484K spike mutations, and the VoC-1 (B.1.1.7) and VoC-2 (B.1.351) variants of SARS-CoV-2.“
So either we truly have a magic game-changer drug, which is Prozac or any other antidepressant, or we are chasing another chloroquine mirage. What is definitely true, that there will now be many people taking those psychopharmaca for no valid reason but some shaky clinical data, in vitro studies and press releases.
And the “happy pill” Prozac is not a harmless drug. Among its side effects are sexual dysfunction, addiction with withdrawal syndrome, QT prolongation (same cardiac side effects as chloroquine), and risk of suicide.
Who cares. Some doctors, like here the US gastroenterologist Farid Jalali, use the pulpit of their medical authority to publicly advocate the use of Prozac and other SSRI right now, on non-hospitalised COVID-19 patients no less, and this is apparently endorsed by Angela Reiersen, whose own JAMA clinical study was neither large nor convincing enough.
On 60 Minutes two weeks ago NIH director Francis Collins seems convinced:
“Fluvoxamine could certainly be something you wanna put in the tool chest. ‘Cause it looks as if it has the promise to reduce the likelihood of severe illness. […]
it’s the FDA who will have the job of figuring out whether to give an approval– for this use of that drug. And it will be about benefit and risk. And the benefit is maybe even a reduction of 20% of the chances that you’re gonna end up in the hospital, that’s probably a good thing.“
Maybe Collins popped some happy pills before he said that.
The Dean of Emory University School of Medicine Vikas Sukhatme and his wife Vidula Sukhatme went much further in their call for action from February 2021. They invite all doctors to do like Seftel and start mass-prescribing fluvoxamine off-label now (“real world evidence“), which they say is better than randomized controlled clinical trials. Other drugs they list as effective are antiparasitics ivermectin and nitazoxanide, anti-inflammatory colchicine and heartburn medicine famotidine. Maybe even in combination, because “real world”?
David Boulware, whose clinical trials previously proved HCQ as useless for COVID-19, told me:
“Fluvoxamine and fluoxetine are interesting possible oral therapies which need further clinical testing to determine their actual effect when started as early outpatient therapy. Lab data and observational data have limitations, but these are starting points to move forward possible compounds to test in randomized clinical trials.“
I am less optimistic.
Update 10.04.2021
Steve Kirsch now commented under this article. I verified that the IP address belongs to him personally. He first wrote:
“Leonis, Pierre Kory and I would be happy to debate you live on youtube. Will you accept?“
Now, Pierre Kory is the US doctor who proselytizes ivermectin as COVID-19 cure (read here). His ivermectin campaign paper on Frontiers has been erased (not just retracted) by the publisher, I hope it was also partly due to my reporting. I asked Kirsch to elaborate on this connection. He did:
“yeah, both the IVM and FLV [ivermectin and fluvoxamine, -LS] evidence is super compelling alone and every doc who has used the combo is amazed at the improvement over IVM alone. So yeah, they go hand in hand.“
But where is Zinc?
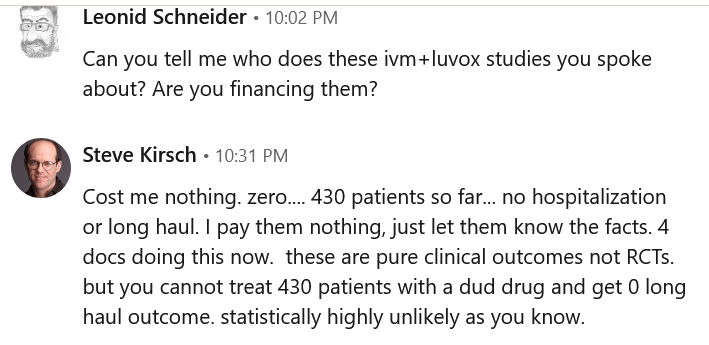
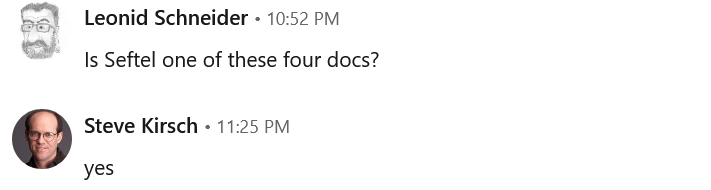
I then contacted Kirsch via LinkedIn. When asked about these ivermectin and fluvoxamine combo treatments he is involved with, the $230 million heavy entrepreneur (who likes to dispense medical advice), declared that 430 patients have been already treated outside of any clinical trial, by four doctors:
“Cost me nothing. zero…. 430 patients so far… no hospitalization or long haul. I pay them nothing, just let them know the facts. 4 docs doing this now. these are pure clinical outcomes not RCTs. but you cannot treat 430 patients with a dud drug and get 0 long haul outcome. statistically highly unlikely as you know.“
He also added:
“With FLV and IVM, we have huge statistical significance alone and in combo.“
David Seftel is one of these 4 doctors, as Kirsch admitted.
Donate!
If you are interested to support my work, you can leave here a small tip of $5. Or several of small tips, just increase the amount as you like (2x=€10; 5x=€25). It#s cheaper than any COVID-19 quack cure!
€5.00

Criticism of the JAMA paper:
http://mathburritos.org/fluvoxamine-challenge-email.html
LikeLike
Pingback: Le parole per dirlo - Ocasapiens - Blog - Repubblica.it
Pingback: Le parole per dirlo – ocasapiens
Another clinical trial with fluvoxamine (plus ivermectin and metformin arms) started recruiting a month ago.
https://www.togethertrial.com/news
https://clinicaltrials.gov/ct2/show/NCT04727424
LikeLike
These guys have it all wrong, it is charcoal that protects against Covid, ha ha!
https://pubmed.ncbi.nlm.nih.gov/33254498/
from the same investigator:
https://pubpeer.com/search?q=joseph+shapiro
LikeLike
Wrong again, let’s forget about charcoal. It is rectal ozone that is the true weapon against covid:
https://pubmed.ncbi.nlm.nih.gov/32838181/
LikeLike
Uhm.
LikeLike
Leonis, Pierre Kory and I would be happy to debate you live on youtube. Will you accept?
LikeLike
How do I know you are really Steve Kirsch?
But I sure am not surprised that fluvoxamine goes together with ivermectin.
LikeLike
Leonid, you can easily DM me on twitter to verify or send me an email on LinkedIn if you want to be sure it is the real me.
And if you want to attach money to the debate, we can have an unbiased audience judge the debate and if you win, it will fund your future work. Since you are completely confident in your statements, this is a no risk proposition for you… However much you want to put up as a wager is fine with me… the more you wager the more you win…. Way better than $5 donations… you can fund your work for years with one debate.
We can have med school students at a top US university be the judge so it will be fair or I’m open to other unbiased options.
It’s going to be more fun if there are actual consequences to losing.
And yeah, both the IVM and FLV evidence is super compelling alone and every doc who has used the combo is amazed at the improvement over IVM alone. So yeah, they go hand in hand.
LikeLike
So your doctor partners now prescribed IVM and FLV as a combo to COVID-19 patients? Dr Seftel, or also others?
LikeLike
When will the debate be? I hope you’re not having second thoughts. I think it would be interesting at least, and perhaps enlightening.
LikeLike
Dr Angela Reiersen:
“I have come to believe that both fluvoxamine and ivermectin are likely beneficial. I am anxiously awaiting upcoming results of the Together trial, an RCT which includes both drugs.”
The investigator himself is sounds skeptical in the interview:
LikeLike
https://nationalpost.com/health/inexpensive-anti-depressant-could-be-best-covid-treatment-yet-canadian-led-trial-finds
Any comments on this now? Looks like it has done quite well in trials or am I missing something?
LikeLike
Ask a doctor. https://twitter.com/josegallucci/status/1425623309362860043?s=20
LikeLike
I was wondering what your thoughts were but okay. I don’t have twitter and don’t speak Portuguese but it seems like he says Ivermectin doesn’t work. Sure I saw that, much like hydroxychloroquine before it. He says to not focus on the Fluvoxamine RRR number of 30% in favor of the ARR which is much lower 4.5%. Do you agree with this? If so what does that say about the vaccines with ARRs that are much much lower than that?
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7996517/
Also this guy is a doctor from the story I linked…
“Dr. Gerald Evans, head of the infectious disease department at Queen’s University’s medical school, said he’d like to see even larger trials conducted in other parts of the world to confirm the findings.
Article content
But Evans noted the trial did back up those earlier studies and was headed by respected researchers. He called the findings “impressive.”
“Everything that I’ve seen does suggest it’s an honest, true signal,” he said. “This is the first drug that has shown a consistent benefit for COVID 19, which separates it from others being studied.””
Why can’t I take his word? Is that twitter guy a better doctor?
LikeLike
Hi,
Ivermectin doesn’t work at all. HCQ is worse, and it has no biological plausibility. Yes, it appears to be a ‘signal’ with Fluvoxamine, but first of all, we need to see the published final results, and we need replication. Avoid jump to conclusions.
ARR is misleading for vaccines. RRR is the “usual scale” considered by the medical community when talking about vaccine efficacy. Why? Because ARR depends on the event rate (the vaccine group has obviously less events) and vaccines trials are design with event-driven analyses.
https://www.medscape.com/viewarticle/950117
https://www.reuters.com/article/factcheck-thelancet-riskreduction-idUSL2N2NK1XA
LikeLike
First of all thanks for the links on ARR and RRR, both are quite good, I’m not sure I 100% agree with the debunking but they make their point and are right that they are complimentary. Secondly I do not like how you presume I thought that Ivermectin or HCQ would ever work and need it explained that it doesn’t. Seemingly if I acknowledge the result in the discussed study on fluvoxiamine is promising that I must for some reason be pushing HCQ or ivermectin, I find that this is very, VERY good insight into just where this criticism comes from. I’ve seen the work on HCQ and now ivermectin, it is pretty clear at this point but that work is not this work though. Finally I understand the importance of both replication and publication.
There is earlier published work on this subject which lead to this study that was also dismissed out of hand on this very page. So it appears they are already covering replication and I’m sure that will continue after this study, in fact with the massive surge of cases in the US right now I’d imagine it is going to get more testing than was planned very quickly as hospitals will be looking for anything to keep people out of beds soon. A lot of places are already filling up or full and we are doing nothing to stem the spread. I fear this wave is going to put our previous waves to shame. I also look forward to seeing the final publication, who knows maybe some massive flaws will pop out there and you can come back and cover them here.
I’ve been a scientist for 20 years, and integrity actually matters to me to the point where I don’t jump to a negative conclusion about a set of work just because I have a beef with those doing it. This includes acknowledging promising early results especially when those results are based on an earlier set of work pointing the same direction. Having a page named FOR BETTER SCIENCE that is looking to actively ignore science when it doesn’t agree to some preformed set of conclusions seems lacking in RESEARCH INTEGRITY and BIOMEDICAL ETHICS in my opinion.
LikeLike
So you say I lack ethics and integrity, but Dr Seftel is a hero? Cool.
Btw, your other hero and sponsor of the Luvox circus, Kirsch, is a big fan of Kory and ivermectin.
LikeLike
Leonid, why don’t you debate Kory and me on Fluvoxamine and Ivermectin. I’ll invite a few others as well like Ed Mills so you can take us down en masse. How about it? We’ll do it in a recorded zoom call that you then agree to post to all your readers to show them how smart you are. How about it?
LikeLike
So sorry to disappoint, Steve, but I fear my English is not good enough. Try Eric Chabriere.
LikeLike
Who said anything about any heroes? I have no idea who Kirsch is although he appears to have responded here. I found this work while looking for answer to long covid symptoms that have afflicted me now for more than a year and SSRI inhibitors were something popped up, leading me to some of the work with fluvoxiamine. I really don’t know the authors or whatever you are on about, I will look into it though. I found your page as part of my search and was initially disheartened again by what I read here. I thought I was once again researching another HCQ type situation that was headed no where. But having seen some of the results it seems like there is something more going on which is why I came back looking for your thoughts after the latest round. I do think your anger/beef with those running this is effecting your perception of the study and yes perhaps compromising your integrity to an extent. I’m sorry if that is harsh. We all need checks sometimes to keep us level. I’m eager to see where this work goes but realize there is still many points it could fail. Who knows perhaps you’ll get the last laugh on it all in the end.
Thank you.
LikeLike
I am sorry to hear of your health problems from covid19. But please don’t let it out on me. Apologies for misunderstanding, I thought you read my article above, including about Dr Seftel.
LikeLike
Pingback: Ivermectin now against COVID-19, because – For Better Science
The antidepressant fluvoxamine has been somehow proven to be the miracle COVID-19 game changer in a phase 3 clinical trial, vouchsafed by the authority of The Lancet.
This was the paper:
Gilmar Reis , Eduardo Augusto Dos Santos Moreira-Silva , Daniela Carla Medeiros Silva , Lehana Thabane , Aline Cruz Milagres , Thiago Santiago Ferreira , Castilho Vitor Quirino Dos Santos , Vitoria Helena De Souza Campos , Ana Maria Ribeiro Nogueira , Ana Paula Figueiredo Guimaraes De Almeida , Eduardo Diniz Callegari , Adhemar Dias De Figueiredo Neto , Leonardo Cançado Monteiro Savassi , Maria Izabel Campos Simplicio , Luciene Barra Ribeiro , Rosemary Oliveira , Ofir Harari , Jamie I Forrest , Hinda Ruton , Sheila Sprague , Paula McKay, Alla V Glushchenko, Craig R Rayner, Eric J Lenze, Angela M Reiersen, Gordon H Guyatt, Edward J Mills Effect of early treatment with fluvoxamine on risk of emergency care and hospitalisation among patients with COVID-19: the TOGETHER randomised, platform clinical trial The Lancet Global Health (2021) doi: 10.1016/s2214-109x(21)00448-4
The world is now screaming that fluvoxamine prevents deaths, but the authors admit it is not the case:
Thus, no significant difference in deaths up until adjustment. Also:
The authors did find a difference somewhere though, once “hospitalisation” was modified:
The TOGETHER trial NCT04727424 was coordinated and sponsored by McMaster University in Canada, plus some charities and a took place in Brazil, and also tested ivermectin, metformin and interferon.
It is worth noting that while the trial may have started independently, its results were published with the significant contribution of the psychiatry professors Angela Reiersen and Eric Lenze of the Washington University, who have been advocating for fluvoxamine as COVID-19 cure since their own studies. Thus, not entirely independent confirmation.
Nobody has a clue how a SSRI antidepressant is supposed to work against a virus infection, but now that we know it prevents COVID-19 deaths and hospitalisations (shut up with your nitpicking!), everyone is busy with making up a mechanism and drawing diagrams.
Wait, the mechanism is of course autophagy, as argued by the psychiatrist and autophagy researcher Theo Rein of the Max Planck Institute for Psychiatry in Munich, Germany, who is concerned his field doesn’t get enough COVID-19 grants:
Rein, T. Harnessing autophagy to fight SARS-CoV-2: An update in view of recent drug development efforts. Journal of Cellular Biochemistry (2021) doi: 10.1002/jcb.30166
As News Medical explained:
That is because Prof Rein found out that depression is actually, bet you didn’t now that, a disease of autophagy in the brain (Gassen & Rein, Frontiers in Psychiatry 2021), and this in turn explains that antidepressants like fluvoxamine must work because they somehow regulate autophagy, simple as that. Prof Rein also argues that ivermectin and artesunate (an artemisinin derivate) are also promising COVID-19 drugs, because surely they also must act on autophagy somehow.
Maybe Prof Rein tries to help a fellow Max Planck Institute director, Peter Seeberger?
In any case, Lancet is not to be argued with. This journal told us that Sputnik V vaccine is 100% safe and 100% efficient, that all talk about COVID-19 lab origins is a conspiracy theory, and that Macchiarini’s trachea transplants saved lives. Because of The Lancet, we all will be taking fluvoxamine. Even if it doesn’t really work against the coronavirus, it will sure lift the mood, so you can die with a smile!
LikeLike